Mapping the harm
Rights-driven gender medicine has thrown off safeguards as it colonises health systems around the globe, but it faces a new challenge
The rise of rights-driven gender medicine and ill-defined laws discouraging exploratory psychotherapy run counter to the welfare of the distressed young people supposedly championed by the “affirmative” worldview.
This is the warning from a landmark paper charting the adoption of the “Dutch protocol” for medicalised gender change of minors across 13 Western nations since 1999, with a weakening of normal safeguards over time in most cases, but also a reassertion of cautious, evidence-based treatment policy begun by Finland in 2019 and followed by Sweden and the United Kingdom.
Australian child and adolescent psychiatrist Dr Kasia Kozlowska is first author of the new paper, with 22 colleagues from a dozen countries, including well-known figures in the gender clinic debate such as Canada’s Dr Ken Zucker, Finland’s Professor Riitakerttu Kaltiala, Sweden’s Professor Mikael Landén, Genspect founder Stella O’Malley, and the French psychoanalysts Dr Céline Masson and Dr Caroline Eliacheff.
The open source paper, published on November 2 in the journal Human Systems: Therapy, Culture and Attachments, notes the emergence of an “unrestricted”, child-led “gender-affirming” treatment approach, “one where many (or all) safeguards have been removed and where puberty blockers and cross-sex hormones—coupled with early social transition—are seen as first-line treatment for gender dysphoria in children/adolescents.”
“[T]he countries that have applied the rights approach unconstrained by other considerations or restrictions have tended to downplay or dismiss questions concerning potential harms—questions that are now being raised by the increasing number of detransitioners.”
Dr Kozlowska and her co-authors challenge the identity-rights affirmative model with the 1989 United Nations Convention on the Rights of the Child, provisions of which would raise “concerns about government legislation that funnels children into experimental treatment that lacks a research foundation and long-term follow-up.”
The authors argue that the UN convention would also question “the widespread use of puberty blockers and cross-sex hormones that are not approved for gender dysphoria by the majority of national drug-regulation agencies and that have likely irreversible consequences for the child’s intellectual (brain) and physical development.”
They observe that the shift to supposedly “child-led” medicine has taken place with the “involvement of powerful pharmaceutical companies,” the intrusion of gender ideology into education and politics, social media influence, and a cultural moment in which the distress of young people is expressed as “gender dysphoria.”
But the very fact of the new paper—and the growing global network of concerned clinicians and researchers reflected by its multiple authors—will spread the news among international health authorities of an emerging evidence-driven consensus view that distressed children are being exposed to experimental medicine.
In contrast to the rights-driven medicalised approach, this “diverging path” taken by the UK, Nordic countries and US Republican states such as Florida, gives priority to patient safety, the doubtful capacity of minors to consent, and the need to elucidate the effects of treatment by employing the gold-standard method of “systematic review” to assess the quality of the scientific literature.
“As [shown by systematic reviews of the evidence undertaken independently in those jurisdictions, the] medically oriented, gender-affirming hormonal treatments are experimental and not currently supported by evidence-based medicine,” the Kozlowska et al paper says.
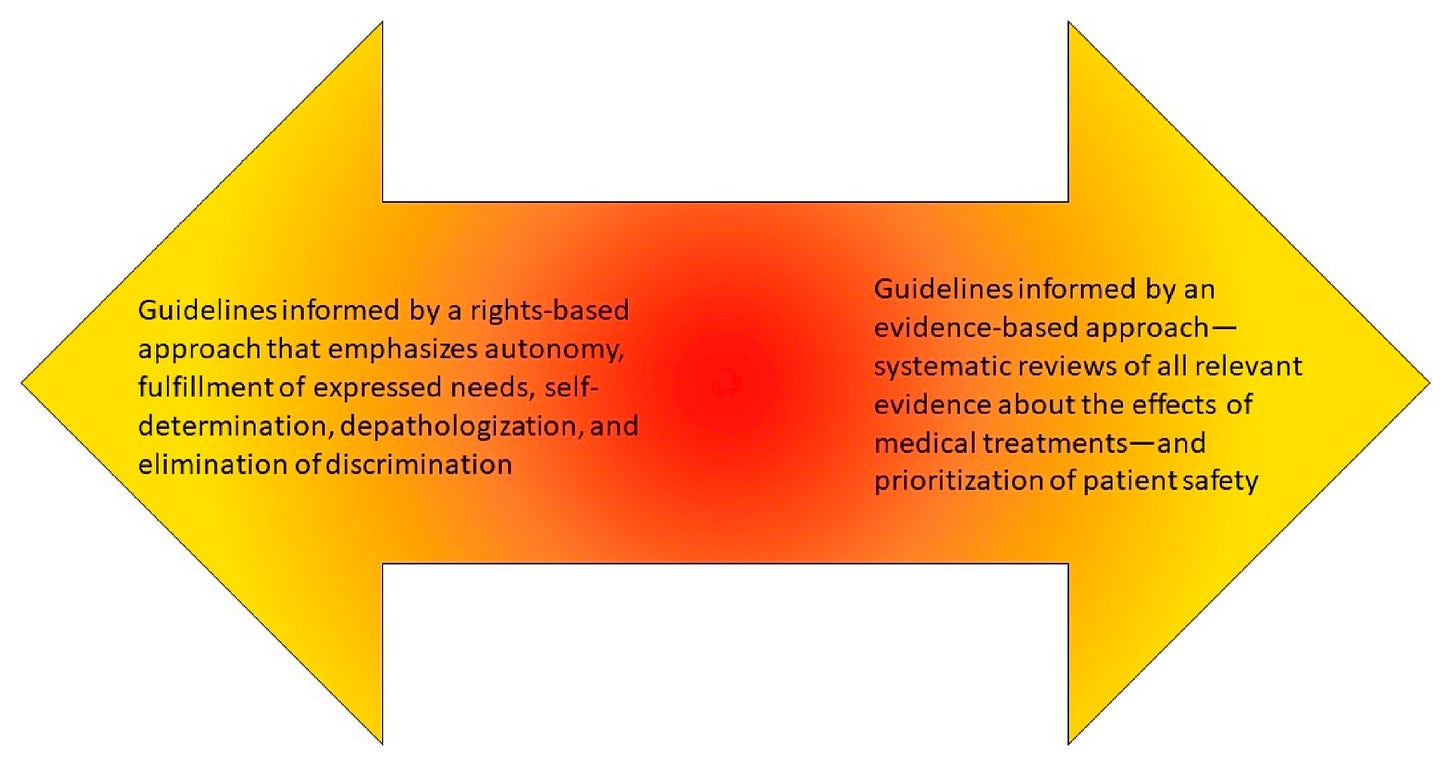
“The interplay—the push and pull—between the rights-based approach and evidence-based approach has created a complex dynamic that will take years to play out, in different countries, and in ways that are hard to predict.
“Whatever the quality of the medical, cultural, and political processes that come to bear on the situation and its challenges, there is likely to be a serious human cost.”
“The [Cass] report repeatedly emphasized the importance of ‘normal clinical approaches to holistic assessment’ and treatment, as used with other young people with complex presentations.
“It emphasizes the importance of psychological and psychosocial interventions to treat and address co-morbid mental health issues, to build resilience, to address family difficulties, to provide ‘more information about gender expressions and the range of possible interventions,’ and generally to ‘explore their concerns and experiences and help alleviate their distress, regardless of whether they pursue a medical pathway or not’.”—Kozlowska et al, journal article, 2 November 2024
Country highlights from the paper of Kozlowska et al—
America | “The Department of Health and Human Services (HHS), a branch of the federal government, has attempted to impose a national mandate that would require doctors and healthcare entities to provide gender-affirming care. The HHS rule intends to prohibit ‘gender identity discrimination.’ Ostensibly, a physician would violate a child’s civil rights if the physician did not transition a child upon request. Currently, there is no other condition for which HHS requires physicians to prescribe off-label medications.” “Currently, at least 79 children’s hospitals provide gender-reassignment interventions [in addition to many other prescribers]… Insurance data suggest that more than 18,000 youth are currently receiving gender-reassignment interventions in the United States.”
France | “Consultations at university-affiliated gender clinics [in France] are conducted by multidisciplinary teams involving ‘somatic doctors’ and psychiatrists. Since 2015, these multidisciplinary consultations have included representatives from transgender associations such as Trans Santé France. During the multidisciplinary meetings, the medico-surgical indications are considered, and decisions are made collectively. Psychotherapeutic follow-up is not systematic… Clinical care can also be sought through a state-funded organization, Le Planning Familial. This organization promotes self-determination and gender affirmation, and facilitates quick prescription of cross-sex hormones at the request of adolescents without assessment or psychological support. Hormonal treatments by private medical practitioners can be delivered on demand after one or two consultations.”
New Zealand | A 2023 gender-affirming hormone guideline for adults (from age 16) in New Zealand does away with the requirement for a mental health assessment and tells doctors not to worry that patients may come to regret treatment. The guideline says: “Some providers may feel anxious about ‘getting it wrong’ or worry that their patient may later regret their decision. The informed consent process outlined in this document respects the autonomy of the patient as a competent adult who has the capacity to make their own decisions about their body and health once they have been given the necessary information. [If the patient decides to stop hormones, this] is not—and should not—be viewed as a mistake or a failure.”
Ireland | Criticism of the safety of the rights-based treatment approach to minors has come from clinicians at Ireland’s adult National Gender Service. In April, following the release of the UK Cass report, Irish Health Minister Stephen Donnelly announced that “a new clinical programme for gender healthcare,” drawing on the best evidence, would be developed over two years.
Canada | “Egale, ‘Canada’s leading organization for 2SLGBTQI people and issues,’ has developed information sheets that describe a broad range of practices as forms of ‘conversion therapy.’ From the perspective of this organization, almost any evidence-based therapeutic practice can be perceived as a form of conversion therapy. [Egale claims that] ‘the lack of treatment or service from a healthcare provider to provide gender-affirming healthcare such as hormone replacement therapy, is also a form of conversion practice’.”
The Kozlowska paper includes a country-by-country table showing the year of adoption of the Dutch protocol; the regulatory status and funding for puberty blockers; notes on any national guidelines; any laws allowing self-declared gender change; any “conversion therapy” bans; and the current treatment approach.
Punishing therapy
Harsh laws prohibiting poorly defined “conversion therapy” have spread rapidly across jurisdictions and critics judge them likely to restrict ethical alternatives to the gender-affirming model with its social and medical transition of minors.
“The neutral stance of exploratory psychotherapy contrasts with the gender-affirmative approach, where verbal affirmation of the child’s expressed gender is the first active intervention,” the Kozlowska et al paper says.
“[B]ecause of the way in which these laws are likely to be worded or enforced, they work against the interests of gender dysphoric children and their families, who may be unable to access the exploratory psychotherapy from a neutral therapeutic stance that is a vital component of evidence-based interventions for such children.
“They may also not be able to access psychotherapy for their co-morbid mental health concerns—suicidal ideation, anxiety, depression and so on—because evidence-based interventions for mental health concerns are misconstrued as forms of ‘conversion therapy’.
“Therapists who provide neutral, conventional, exploratory therapy, which is mandated by professional ethics—and by evidence-based guidelines in Finland, Sweden, and the UK—are consequently unable to address the needs of gender dysphoric youth. The legal and professional risks are simply too great.
“The ultimate consequence is that children who might well profit from a neutral therapeutic space may find it difficult to find a therapist who will take them on; instead, they will find themselves channelled to seek care from practitioners who take a ‘gender-affirming’ position and who regard hormonal interventions—coupled with early social transition—as the preferred and first-line treatment for gender dysphoria.”
Graphic: the Kozlowska paper visualises treatment approaches as a spectrum, and highlights the variation within rights-driven and evidence-based approaches, as well as within countries
Pre-empting identity
The Kozlowska paper also points out that the gender-affirming dogma of a stable “gender identity” in minors defies a basic principle of psychiatry that “adolescence is the most important developmental phase of identity formation, and that identity consolidation is the outcome of successfully completed adolescent development.”
“Against this background it was problematic to assume that one facet of identity development—namely, gender identity—would be sufficiently consolidated in early adolescence to justify [medical] interventions on healthy bodies.”
The paper notes that most countries adopted the Dutch protocol for “juvenile transsexuals” without any long-term data and at first insisted on multidisciplinary teams and comprehensive assessment of potential patients in order to mitigate risk.
“The overarching idea was that in the absence of an adequate evidence base, biopsychosocial practice—best practice in paediatrics and child and adolescent psychiatry—was the best means of protecting patient safety.”
And yet—despite an unprecedented surge in patient numbers and a new, chiefly female profile with mental health issues predating any gender distress—the safeguards of formal diagnosis and wholistic assessment were progressively weakened in the name of depathologisation, autonomy, demand-driven healthcare, and anti-discrimination.1
“Our perspective makes [it] apparent that clinical practice in services whose guidelines are shaped by the rights-based approach has shifted away from holistic biopsychosocial practice,” the Kozlowska paper says.
“In many such services, the role of mental health professionals has moved away from the task of conducting comprehensive diagnostic biopsychosocial assessments to providing optional advice and support.”
In “extreme” forms of the rights-driven model, the paper says “gender-reassignment interventions may take place without evaluating the child’s/adolescent’s gender identity, without a biopsychosocial assessment (including no psychiatric evaluation), and without parental consent.”
Under the “extreme” variant of the evidence-based approach, “gender-reassignment interventions for minors may remain largely unavailable because the long-term outcome evidence is considered inadequate to demonstrate their safety and effectiveness.”
The paper by Dr Kozlowska and her colleagues remarks that the new evidence-based treatment policy adopted in a number of European countries gives emphasis to—
“…the importance of the holistic biopsychosocial assessment and treatment, including the provision of a diagnosis of gender dysphoria and the assessment and treatment of co-morbid mental health concerns; the importance of exploratory psychotherapy from a neutral therapeutic stance as the first step in treatment; and legislation or national guidelines that delay access to gender-reassignment surgeries until legal adulthood.”
It is not uncommon to hear gender-affirming clinicians assure a mainstream audience that they undertake comprehensive assessment before prescribing hormones to minors. In other contexts, clinicians may downplay the need for a formal diagnosis or dismiss a mental health assessment as “pathologising.” England’s Cass review included an evaluation of major international treatment guidelines. In her final report, Dr Cass says: “Despite the agreement within the international guidelines on the need for a multi-disciplinary team, and some commonalities between them in the areas explored during the assessment process, the most striking problem is the lack of any consensus on the purpose of the assessment process.”



In 1936, near a century ago, serious mental health conditions in otherwise physically healthy individuals were treated with an experimental surgical procedure. The Frontal Lobotomy, pioneered by António Egas Moniz, a Portuguese neurologist, involved drilling a hole in the skull and severing the nerve connections to the frontal lobes of the brain.
Moniz's work was initially viewed as a breakthrough in the treatment of serious mental health disorders, earning him the Nobel Prize in Medicine in 1949.
At that time innovative/experimental medical interventions did not require the rigorous evidence of efficacy and safety that is mandated today (aka: evidence base). This delayed the realisation that the frontal lobotomy often did more harm than good. Some patients died either during or after the procedure, or were left in vegetative states unable to care for themselves. The last such procedure was performed in the United States in the early 1960’s. The lobotomy epoch is now viewed as a shameful stain on the medical profession.
Fast forward to 2024:
Here we are, 88 years after the Moniz's ‘breakthrough’, our major paediatric teaching hospitals are treating a mental condition in otherwise healthy children with an invasive, irreversible, mutilating, sterilising surgical and hormonal cocktail that is devoid of an evidence base.
Drilling a hole in the skull and severing connections with the frontal lobe of the brain doesn’t seem such a bizarre undertaking when compared with concept and practice of ‘gender transition’ of children
(Note: A diagnosis of gender dysphoria is included in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, or DSM-5.)
Well done! More evidence for a more cautious therapeutic.approach is nevertheless still needed.