Non-binary scalpel
Australia's plastic surgeons want universal public funding for "gender-affirming" operations

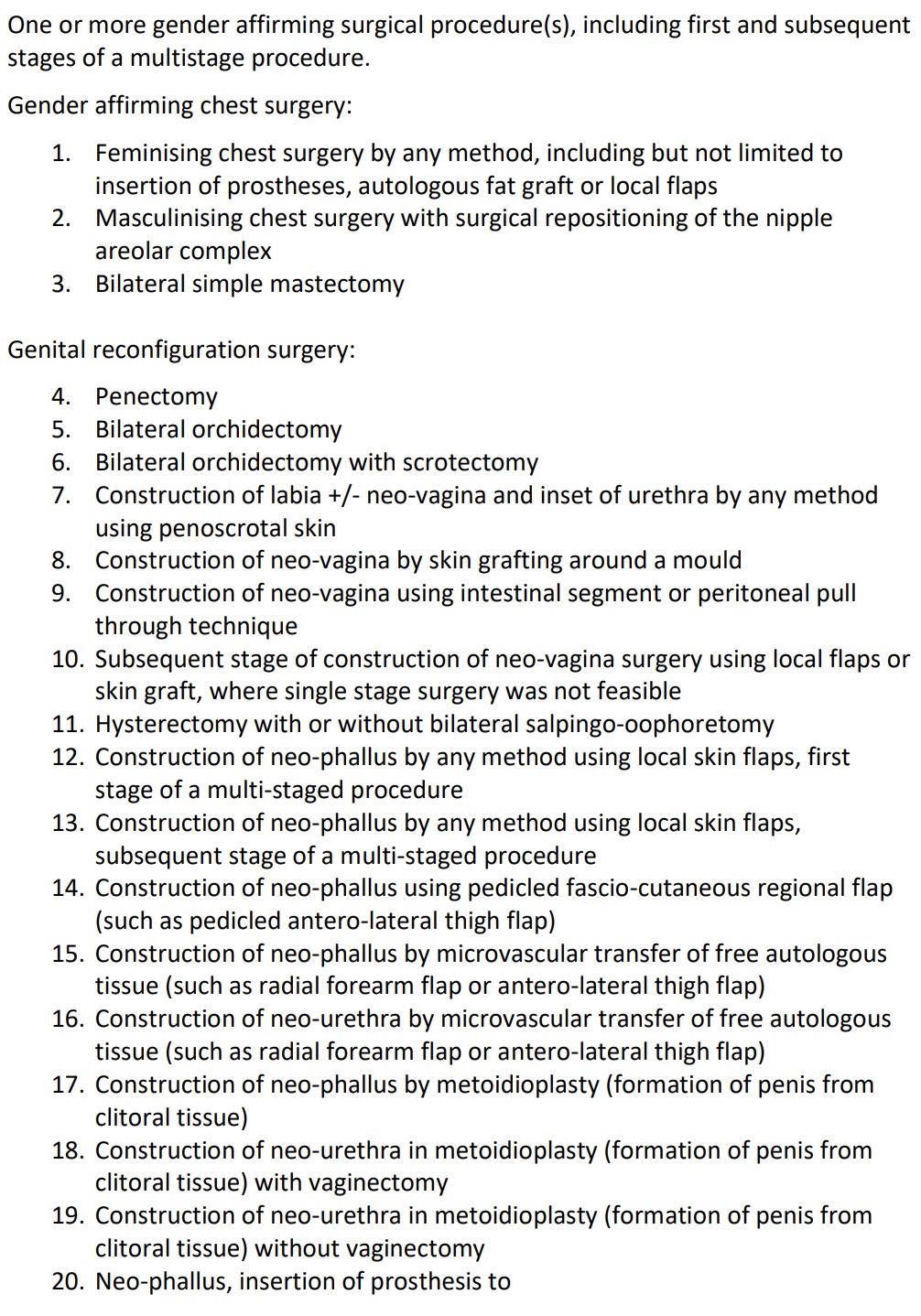
“Non-binary” people who suffer no distress in their bodies should be allowed access, without mandatory mental health screening, to a suite of 28 “gender-affirming” surgeries subsidised by Australia’s taxpayers, according to an application to the federal government.
The operations on the wish list from the Australian Society of Plastic Surgeons include radical procedures to create a pseudo-penis for transgender-identifying females, and to use a section of the colon to fashion a neo-vagina for males whose genital growth was stunted by puberty blockers in childhood.
The outcome of the society’s application, which has been in the works since 2023, will not be known until after Saturday’s federal election. The clinical evidence was considered earlier this month, with the verdict unknown until after a financial analysis yet to come. A recommendation will then be put to Australia’s federal health minister following these deliberations by expert advisory committees and consultation rounds.1
In December last year, current minister Mark Butler was briefed by health officials that “top surgery”—double mastectomy for females or breast implants for males—“can significantly improve a person’s confidence and comfort with their body, helping to reduce feelings of distress related to gender dysphoria.”2
There is no high-quality evidence to support this claim. In Australian jurisdictions and overseas, regretful detransitioners including young adults have launched court actions against their doctors.
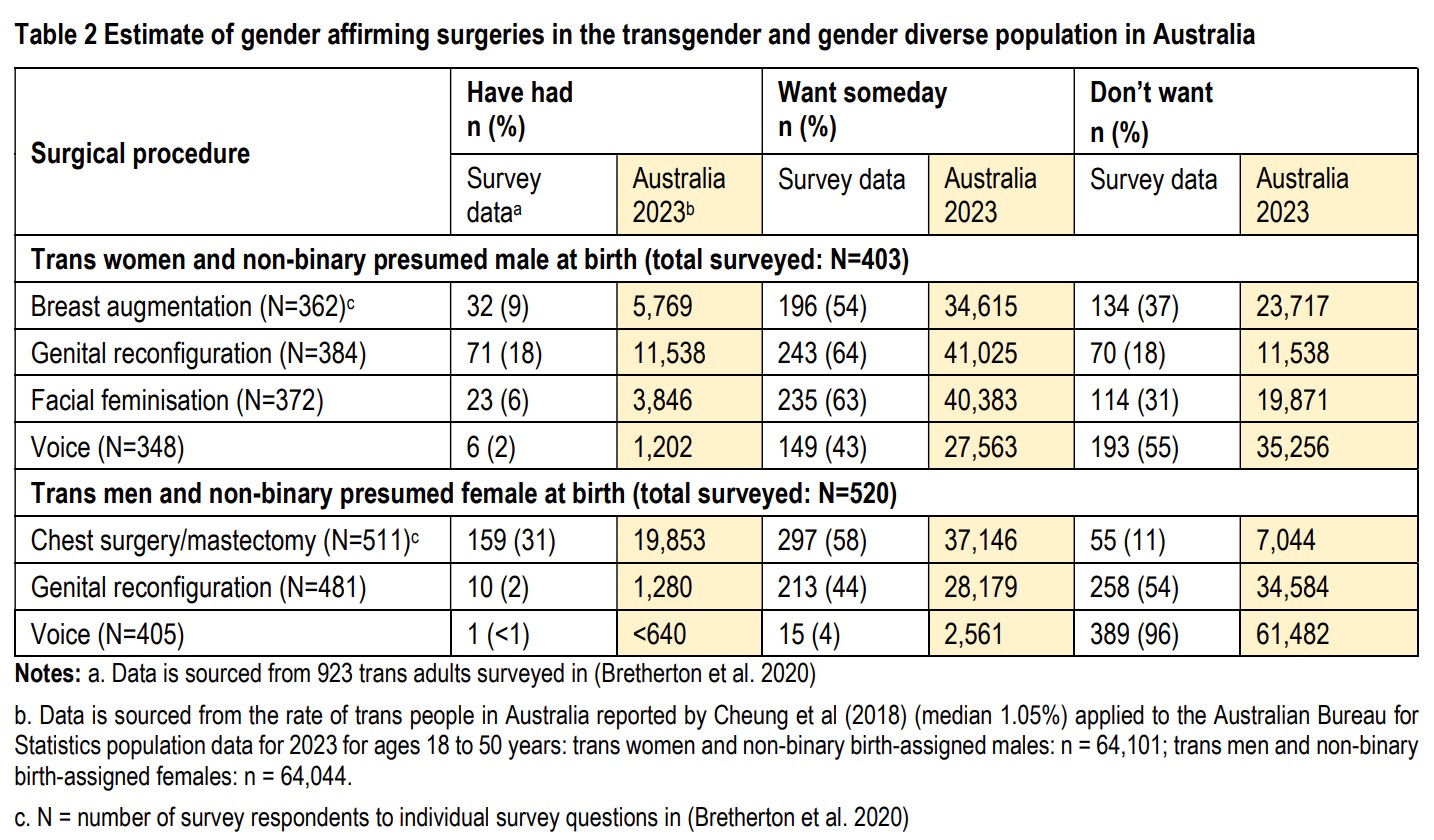
The proposal by the society of plastic surgeons includes an estimate that in a given year, more than 37,000 trans-identifying adult females would want a double mastectomy “someday,” while more than 34,000 males would seek “breast augmentation” in the future.3
It also says that some 30 per cent of people under the trans umbrella are thought to identify as non-binary.
In the UK, the vast majority of the 3,490 gender-distressed patients referred for trans mastectomy from 2021 to 2023 by the NHS were reportedly young women aged 17-25, when the brain has yet to fully mature.
Public documents filed by the Australian plastic surgeons do not reveal the extent of the subsidy being sought by the society, but do include the claim that patients currently funding their own gender surgery face costs up to $50,000.
Graphic: Gender surgeries in search of public funding. For the full list of procedures proposed by the plastic surgeons’ society, see P2 here
What are we treating?
Although the application form requires description of the “medical condition” to be treated, the society argues the only prerequisites for access to these surgeries should be legal adulthood and sustained “gender incongruence,” a term for a sense of disconnect from birth sex that may not involve any of the distress of gender dysphoria.
“There are no specific tests or criteria proposed to determine a person is a candidate for gender affirming surgery,” a key supporting document states.
In commentary on the application, an expert advisory committee involved in the approval process pointed out there are “no detailed diagnostic criteria to assist clinicians in making a diagnosis [of gender incongruence], or to define the duration of sustained gender incongruence.”
Gender dysphoria appears in psychiatry’s diagnostic manual, but gender incongruence is a “depathologised” concept found in the sexual health section of the World Health Organisation’s ICD system.
To bolster its case for public funding, the plastic surgeons’ society emphasises the high rates of mental health disorders, autism, ADHD, and eating disorders in the trans population, but proposes that the opinion of just one general practitioner (GP) should be enough to diagnose gender incongruence and refer patients to surgeons without any requirement for psychiatric or psychological assessment.
However, the GP “will need to rule out other causes of apparent gender incongruence which may occur as part of an acute psychotic episode, or cases where surgery is sought for reasons other than the alleviation of gender incongruence.”
The expert committee cautioned that “not all GPs may be qualified” for this differential diagnosis and favoured the involvement of a multidisciplinary team.
The rights-driven gender-affirming approach tends to favour fast-tracking access to treatment in primary care, while downplaying the need for specialist screening as an exercise in “gatekeeping.”
The committee sent mixed messages on the novel idea that gender surgery no longer depends on the binary logic of “male-to-female or female-to-male” and that the rise of the amorphous non-binary profile makes medical interventions “an individual matter, stemming from [each person’s] own experienced gender.”
On the one hand, the committee expressed the view that non-binary people who do not “choose to dress as the alternate gender or use hormonal therapy” should not “inadvertently” be excluded from access to taxpayer-subsidised surgery.
The society’s list of surgeries includes creation of a neo-penis from a female’s clitoral tissue with or without removal of her vagina.
In Canada last month, a court ruled that a trans-identifying male, known as KS, is entitled to public funding for surgery to create a pseudo-vagina while preserving his penis. KS reportedly does not identify as fully female or fully male.
With the Australian surgeons’ proposal for funding under the public Medical Benefits Schedule (MBS), the expert committee warned that multiple surgical revisions “undertaken when a more extreme cosmetic outcome is desired, rather than for a medically indicated correction, may not fall within the rules of the MBS.”
And the committee said the descriptors for the new MBS surgery item numbers “should clearly differentiate where there is a clinical or functional need for a service, versus where the service might be considered cosmetic.”
The procedures covered by the application include costly facial surgery, and the removal and remodelling of the genitals, with some operations damaging fertility and sexual function as well as involving high rates of complications and demanding surgical “revision.”
Graphic: Estimates of demand for gender surgery, presented by the society of plastic surgeons, and drawing on an anonymous online survey of 928 people
Only the elect
The society of surgeons’ proposal—which cites gender medicine lobbies the Australian Professional Association for Trans Health and ACON, a former gay rights organisation—repeatedly refers to the subset of trans or non-binary people who “wish” or “elect” to “pursue” surgery, with no indication what sets them apart from those who do not opt for bodily modification.
Some of the 28 procedures in question are already available on the MBS, but the society argues that without universal public funding of gender surgery many patients will have to pay to go private or overseas.
The financial impost on the MBS is said to be justified by better “health-related quality of life” and psychological benefits such as a lower risk of suicide but, under the approval process, the question is, compared to what?
The “comparator” chosen for the newly subsidised treatments is a scenario in which no gender surgery is available.
This choice of comparator was strongly contested by opponents of the society’s application who made submissions during consultation.
They argued that “psychological therapy for gender incongruence to help the person become comfortable in their own body should be the comparator” against which the surgeons’ proposal should be judged.
A consultation summary said: “The consumer feedback unsupportive of gender-affirming surgery all raised the concerns that gender-affirming care is often provided without a robust diagnostic process or long-term psychological therapy to address co-morbidities and potential reasons for experiencing gender incongruence such as internalised homophobia, body dysmorphia, neurodiversity and other trauma.”
Other points raised by critics included—
“Concern that there is insufficient good quality research to indicate that surgical treatments improve mental health outcomes or lessen suicidality.
“Possibility for grief or regret post-surgery and the absence of publicly funded reversal surgery.
“Concern that some patients view hormonal and surgical interventions as the solution to their distress. Some patients can suffer tunnel vision and focus on gender surgery as a strategy to avoid thinking about the complexity of their feelings regarding their body, their relationships, their adverse life experiences, and their current life challenges.
“Concern that adolescents and young adults will be eligible for surgery and are vulnerable populations not yet able to adequately consider the long-term consequences and risks of gender affirming surgery.”
The Australian Medical Association and the Royal Australasian College of Surgeons supported the application, but the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) opposed new subsidies available only to one group of people, being those with gender incongruence.
“RANZCOG considered that equivalent funding needs to be made available for intersex and ciswomen living with complex gynaecological presentations.”
The proposal of the surgeons’ society cites a claim by the Trans Health Research group at the University of Melbourne that studies confirm a “link” between “lack of access to safe gender-affirming surgery, and poor mental, physical, and social health outcomes.”
However, Dutch and Swedish research suggests that regret after gender surgery may take 8-11 years to surface. The 2011 Dhejne study, important because of its comprehensive and long-term nature, found that the suicide rate after “sex reassignment” surgery was 19 times higher than in the general population.
Other more recent, comprehensive studies in Finland involving young adults suggest that current patients have high “psychiatric needs” even after medical intervention and that it is their co-morbid psychiatric disorders, not gender distress itself, that drives suicide risk.
The first systematic review and meta-analysis of psychological and physical outcomes for double mastectomy in gender dysphoric females aged 25 and younger has found the evidence base to be of “low to very low certainty.” However, some of the studies under review provided “high certainty” evidence for the outcomes of death, necrosis, and excessive scarring.
This landmark review, published in the journal Plastic and Reconstructive Surgery last September, is not included in the references cited by the public documents in support of the MBS changes proposed by the Australian plastic surgeons’ society. Nor are the sobering studies from Finland and Sweden referenced.
My coverage of the plastic surgeons’ proposal focuses mostly on the document known as the “PICO confirmation” and commentary by the PICO Advisory Subcommittee. This document sets the scene for consideration by the Medical Services Advisory Committee (MSAC), which makes recommendations to the federal government. On April 3-4, MSAC looked at the clinical evidence for the surgeons’ proposal. The result will not be known until a future MSAC meeting has also weighed the financial effects of the proposed changes to the Medical Benefits Schedule. More detail is here and here.
The minister’s office requested an urgent brief following the decision last December by UK Health Secretary Wes Streeting to impose an indefinite ban on private prescribing of puberty blockers. Mr Butler’s officials appear to be relying on a flawed 2024 review by the Sax Institute, which offers both concessions that the evidence base for gender medicine is of low quality and vaguely positive statements favouring its continued practice. I obtained the ministerial briefing under Freedom of Information law.
The activist site TransHub, run by former gay rights body ACON, says the out-of-pocket cost for top surgery ranges from $4,000 to $18,000; from $5,000 to $40,000 for facial surgery; and from $8,000 to $80,000 for genital surgery.


An absolute abuse of public funding.
The list of services funded by Medicare that most of the population want - shorter hospital waiting times, dental care for all under Medicare , just for starters - should be the priority.
Especially when ghouls in the medical profession KNOW surgeries don’t meet even the lowest bar in “First do no harm” and medical ethics.
Saving the announcement till after the election hints at capitulation to a lobby group rather than doing what’s right for ALL Australians.
REALITY: Eight studies suggesting that ‘transition’ is not always a bed of roses:
Risk of Suicide and Self-Harm Following Gender-Affirmation Surgery:
Individuals who underwent gender-affirming surgery had a 12 fold higher suicide attempt risk than those who did not.
2 Long-Term Follow-Up of Transsexual Persons Undergoing Sex Reassignment Surgery: Cohort Study in Sweden (1973-2023):
Persons with transsexualism, after sex reassignment, have considerably higher risks for mortality, suicidal behaviour & psychiatric morbidity than the general population.
3 Trends in suicide death risk in transgender people: results from the Amsterdam Cohort of Gender Dysphoria study (1972–2017):
The suicide risk in transgender people is higher than in the general population and seems to occur during every stage of transitioning.
4 Suicide Mortality Among Adolescents in Finland (1996–2019):
Gender dysphoria alone did not predict mortality or suicide among adolescents referred to gender identity clinics. Psychiatric comorbidities were the primary predictors of mortality. Medical gender reassignment did not mitigate suicide risk.
5 Somatic Morbidity and Cause of Death in Denmark (1978–2010):
Individuals who underwent SRS, somatic morbidity increased from 19% pre-surgery to 23.2% post-surgery, with a mortality rate of 9.6%. The average age at death was 53.5 years.
6 Examining gender-specific mental health risks after gender-affirming surgery: a national database study:
From 107 583 patients, matched cohorts demonstrated that those undergoing surgery were at significantly higher risk for depression, anxiety, suicidal ideation, and substance use disorders than those without surgery.
7 Suicide-Related Outcomes Following Gender-Affirming Treatment: A Review:
From 107 583 patients, matched cohorts demonstrated that those undergoing surgery were at significantly higher risk for depression, anxiety, suicidal ideation, and substance use disorders than those without surgery.
8. Examining gender-specific mental health risks after gender-affirming surgery:
Gender-affirming surgery, while beneficial in affirming gender identity, is associated with increased risk of mental health issues.