Breaking the chain
Low-quality gender research abuses the trust that good medicine demands
Dr Julia Mason
There’s a well-recognised lack of solid medical research on how best to care for children with gender dysphoria. No one has conducted a controlled clinical trial. All we have is low-quality evidence that normally would not be appropriate for guiding medical decision-making, especially when the interventions are irreversible and carry a heavy medical burden. But, for some reason, in this area of paediatric medicine, not only is poor evidence allowed, it’s heavily promoted by major medical organisations.
I want to talk to you about the broken chain of trust in medicine. When you study medicine, it quickly becomes obvious that the amount of information needed to successfully treat patients is massive. So, you have to trust that someone has done the research, that a group of thoughtful, rational people have taken the time to determine what is the best course of action. As a student, you don’t have time to read the original papers that back up the treatment plan you’re being taught.
Dr Steven Levine, [professor of psychiatry and an authority on gender dysphoria], talked about this in his January conversation with psychotherapists Stella O’Malley and Sasha Ayad. He said that before he started medical school, he went to a pre-medical conference, and a professor held up a massive book and said, “This is the textbook of medicine—90 per cent of it is wrong, but I can’t tell you which 10 per cent will still be the truth in 20 years.”
Dr Levine then described young doctors and psychologists confidently telling him exactly how gender dysphoria is to be treated. They were confident because this is what they were taught in medical school or graduate school. They were operating based on 100 per cent trust.
I had the good fortune to start medical school on a Medical Scientist Training Program fellowship. My plan was to get an MD and a PhD in nutrition, and then teach nutrition to medical students. That didn’t happen, which is a whole other story. But I did get to look at medicine a little differently, due to having breaks in my medical education during which I was being a graduate student, instead of a medical student. I spent time in the part of the system that generates the data and eventually the treatment plans. I wasn’t just force-fed 1,000 plans and told to memorise them.
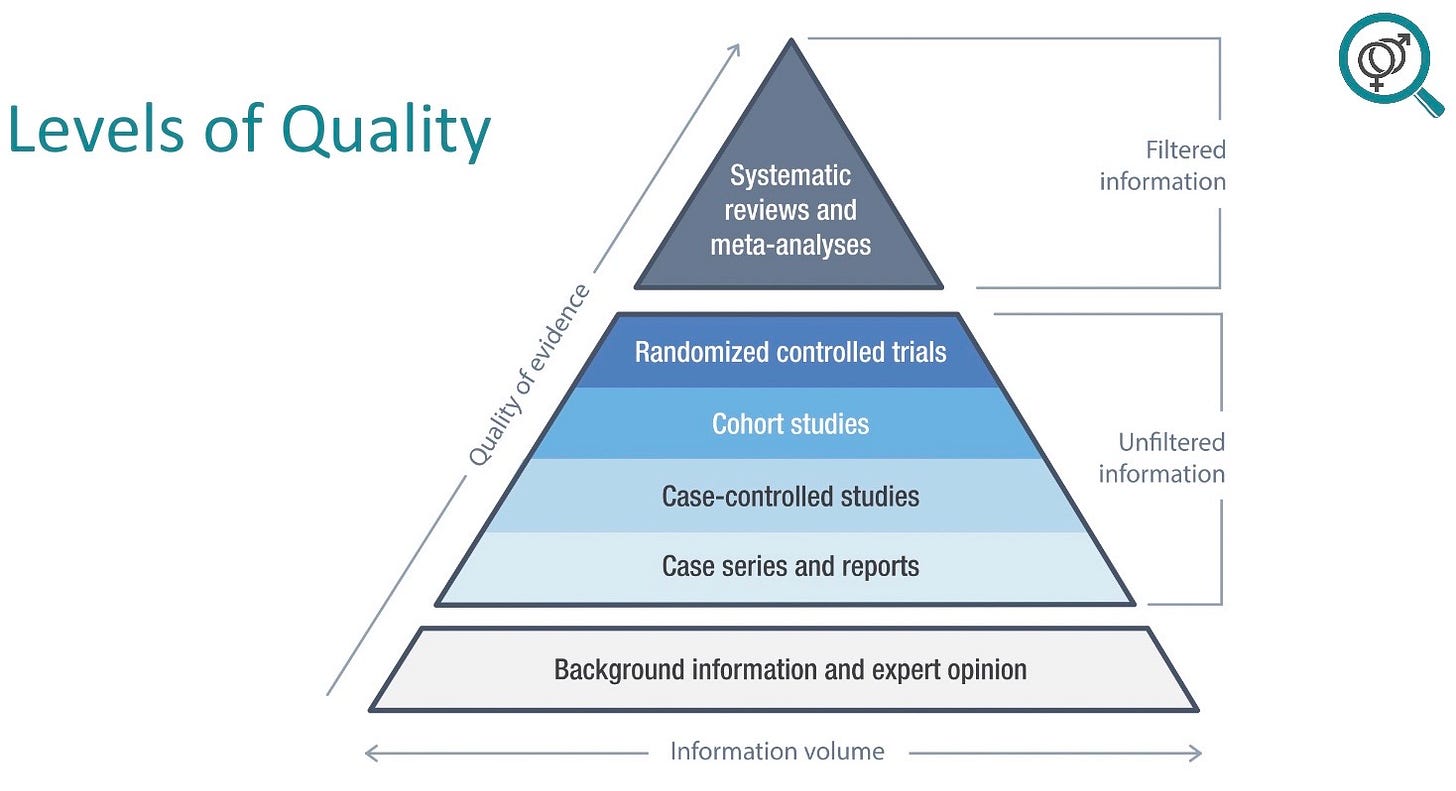
If you are trying to decide whether a treatment plan is supported by evidence, you need to evaluate the evidence. And this is the thing that working paediatricians, for example, don’t have the time or the inclination to do. The lowest level of evidence, the lowest quality of evidence, is expert opinion. This still controls a lot of what happens in medicine, but it’s eminence-based, not evidence-based. The middle levels of evidence consist of case series or reports, then case-controlled studies, then cohort studies, then randomised controlled trials. The highest quality evidence is derived from systematic reviews of the evidence and meta-analyses.
In the case of gender dysphoria, systematic reviews of the evidence have been performed by the National Institute for Health and Care Excellence in the United Kingdom and by the national health authorities in Finland and Sweden. All of these countries subsequently put a halt to immediate “affirmative care” for minors after doing a systematic review of the evidence, because each of these reviews found that the evidence supporting paediatric gender transition is just not there.
And yet, every major medical organisation in the United States will swear up and down in a court of law that the science on this is settled. And the vast membership of the American Academy of Pediatrics, my professional organisation, has been shielded from my dangerous opinions and requests.
None of us have the brainpower to truly, deeply understand why what we do with our patients works. Medicine is littered with the detritus of treatments that we thought were appropriate, like bedrest for back pain, or diet changes for ulcers.
As for paediatric gender medicine, the basis for the practice was laid out in what we often call the Dutch studies. In 2014, Dutch clinicians published a paper on their new method for treating gender dysphoria in young people, in which adolescents were medically transitioned to appear as the opposite sex. Their published group was comprised of the first 70 completer patients—you might start thinking about some bias there—out of which outcomes were reported for the first 55 that basically survived to the end. For some measures, the Dutch reported on as few as 32.
Their measurement of gender dysphoria with a sex-specific questionnaire—the Utrecht gender dysphoria scale—was completed by 33 people. And then they flipped the scale at the end of the study, and they started asking the natal males about their periods, and the natal females about their erections. I’ve always said, I could take a gender-dysphoric kid, give them a fetching hat, and tell them that it totally makes them look like the opposite sex, and then administer the opposite-sex gender dysphoria scale, and I would get significant results.
The 15 non-completers included three people who developed morbidity which prevented them from continuing, two people who refused to take part, one person who medically detransitioned, and one person who died from post-surgical sepsis as a direct result of their transition. Keep in mind that these cases were excluded from consideration when the Dutch reported their modest improvements in this uncontrolled and unscientific study of major medical interventions. To this day, the Dutch study represents the strongest clinical evidence for the supposed benefits of adolescent medical transition.
Data recycling
More recently, we’ve been told that puberty blockers prevent suicide in young people with gender dysphoria. The 2020 paper promoting this idea—titled “Pubertal suppression for transgender youth and risk of suicidal ideation”—is based on a poor-quality convenience-sample survey, the 2015 U.S. Transgender Survey (USTS), a mostly online survey that offered cash prizes for participation. This was a political survey created by the National Center for Transgender Equality. It was not designed for medical research. It was a lobbying document. Participants were recruited through transgender advocacy organisations or social media and were asked to promote the survey among their friends. This recruiting method yielded a large, but highly biased sample. The experiences of detransitioners were not included. Transitioned people who are not politically active were also under-represented in this survey.
There’s good evidence that the 2015 USTS is not representative of the American population who identify as transgender. The quality of the data is also highly suspect. For example, 73 per cent of the respondents who reported taking puberty blockers said they started them after age 18, which seems unlikely, as most young people have finished puberty by that age. Finally, this data set, this snapshot in time, makes it impossible to determine causation between linked factors. We can’t decide if puberty blockers prevent suicide from this study. Despite this, the idea that puberty blockers save lives has become the dominant narrative in both the popular press and medical journals.
Multiple rebuttals to this 2020 USTS-derived paper were submitted, pointing out flaws, but the journal—Pediatrics, the official journal of the American Academy of Pediatrics—refused to correct the paper or even acknowledge the letters by publishing them. The same survey has been used by Dr Jack Turban [an American psychiatrist popular with media outlets who was first author on the Pediatrics article] for at least six other papers on topics ranging from trying to prove that psychotherapy is harmful, to asserting that surgery is extremely helpful. None of the rebuttals to any of these papers have been published by these journals.
Stifling debate breaks the chain of trust. Busy doctors don’t have time to evaluate the quality of the research. We trust the journals to vet the research they’re publishing and to platform debate. For me, the final straw was when Pediatrics selected the Turban et al article as their number one paper of the year in 2020.
I wrote to the journal editor and his first response was that the Turban et al paper was selected because it got the most clicks. Then he told me that I should submit a “Pediatrics perspective”, sharing my concerns. I followed his advice. I wrote a paper called “Far from settled science: a call for caution in the care for gender-dysphoric youth”, based on my experience with multiple transitioning teenagers, none of whom were thriving. I expressed concern about what’s happening with paediatric medical transition and talked about the lack of evidence supporting it.
Per the usual process, my article was sent out for peer review. I expected pushback, but I didn’t expect what I got. I had all these points about what worried me. And then I referenced the developmental issue of socially transitioning young children, by saying children are likely to believe that the doctors can actually change their sex when they grow up. We can’t, and it’s cruel to imply that we can. The reviewers had a big issue with this statement. Apparently, the first reviewer thinks that we do change the sex of our patients. And the second one was worried that my assertion would offend children who read medical journals.
Needless to say, my paper was not accepted for publication. It’s not just my paper getting banned, researchers have submitted dozens of papers and rebuttals without success. The top-tier journals who promote these notions [about paediatric transition] are unwilling to publish our rebuttals. Of course, we have had success getting our rebuttals into other high-quality journals, but unfortunately, they’re not widely read by paediatricians.
One paper on which I am co-author—“Reconsidering informed consent for trans-identified children, adolescents and young adults”—was sent out to multiple reviewers. Of course, after it was published, the same journal published four commentaries, two relatively friendly, one snide and one fairly hostile. Which is great, this is how science is supposed to advance with open debate.
But back to what happens in gender world. Last year brought a paper by researcher Dr Diana M Tordoff et al with the title “Mental health outcomes in transgender and non-binary youths receiving gender-affirming care.” Journalist Jessie Singal summarises the situation in his headline, “Researchers found puberty blockers and hormones didn’t improve trans kids’ mental health at their clinic. Then they published a study claiming the opposite.”
This paper is amazing, amazing that it got published. Basically, the researchers followed a few dozen patients through their experiences with their gender clinic, and found that the patients getting affirmative care didn’t have significantly improved mental health scores. But hey, the untreated kids got worse, at least the ones that stuck around, so if you squint and run some fancy statistics, you can posit that the treated kids would have also gotten worse. So the fact they stayed pretty much the same is actually an improvement. Seriously, that’s what it says.
It’s not how this paper was presented to the public. The press release declares: “Gender-affirming care dramatically reduces depression for transgender teens, study finds.” The first sentence reads, “[University of Washington] Medicine researchers recently found that gender-affirming care for transgender and non-binary adolescents caused rates of depression to plummet.” And that’s pretty much how things go in the super special world of paediatric gender medicine. Null results get magicked into positive results. And everybody knows that “affirmative care saves lives.”
Here’s another example. In 2022, researcher Dr Mona Ascha et al published a paper on chest-masculinization mastectomy on 14-24 year olds, but had only a three-month follow-up and a 14 per cent drop-out rate. Their conclusion is that, “Top surgery [mastectomy] is associated with improved chest dysphoria, gender congruence and body-image satisfaction in this age group.” Conspicuously missing from the list of significant results are things like rates of depression, anxiety, life satisfaction, or other useful psychological measures. The chest dysphoria scale is a lot like the Utrecht gender dysphoria scale. If you remove someone’s breasts, at their request, the score is going to improve.
Nevertheless, in this paper, the researchers claim that their findings would “help dispel misconceptions that gender-affirming treatment is experimental.” The paper was accompanied by an editorial—this is the journal JAMA Pediatrics—entitled “Top surgery in adolescents and young adults: effective and medically necessary.”
Another recent paper, by Dr Diane Chen et al, is from the big long-term project we’ve been waiting for, because they got big bucks from the National Institutes of Health. They had to describe what they planned to do with the money. They said they would look at eight things: gender dysphoria, depression, anxiety, trauma symptoms, self injury, suicidality, body esteem and quality of life. In this paper, the researchers report on depression and anxiety, and they don’t have awesome results. And they don’t report on the other six outcomes. They had a massive drop-out rate of 30 per cent in just two years, and two out of 315 patients died from suicide, which is a stunningly high rate. These are kids being affirmed at what’s supposed to be the best gender clinic in the country.
So we need to be following the evidence, not self-declared experts. We are engaging in a massive uncontrolled medical experiment on children. In fact, it’s not even an experiment because most clinics aren’t collecting any sort of follow-up data. We don’t know why so many young people are identifying as trans. And we know even less about how best to care for these children. The chain of trust has been broken in the field of paediatric gender transition. Everybody knows that “gender-affirming care is life-saving care,” except that nobody has actually shown this to be true.
The Society for Evidence-based Gender Medicine is one of a few organisations fighting for transparency in gender medicine and to restore the integrity of the scientific process in the field of gender medicine. Unfortunately, our well-reasoned attempts are frequently met with accusations of “transphobia.” Every week more and more clinicians reach out to us and our ranks are growing.
This is an edited extract from Dr Mason’s April 29 presentation “The broken chain of trust” at Genspect’s Bigger Picture conference in Ireland.
Dr Mason is a founding board member of SEGM, an international group of doctors, researchers and academics. She completed her paediatric training at Children’s Hospital Los Angeles in 1997.
More reading—
Abbruzzese et al, “The myth of ‘reliable research’ in pediatric gender medicine: a critical evaluation of the Dutch studies—and research that has followed”
Levine et al, “Reconsidering informed consent for trans-identified children, adolescents, and young adults”



Dr Mason’s summary of the litany of contradictions that are somehow used to justify this invasive irreversible mutilating medical procedure in young people leads one to the believe that many of the sacred tenets of medical practice have been put on hold.
To add, I cite text from a recent edition of the US ‘Current Sexual Health Reports’, a journal with the defined objective of “providing the reader, in a systematic manner, with the views of experts on current advances in the sexual health field in a clear and readable manner”:
The evidence base for gender-affirming interventions is sparce and of very low quality. While the evidence of benefits is highly uncertain, the harms to sexual and reproductive functions are certain, and many uncertainties about the long-term health effects exist. As a result, it is hard to ethically justify continuing to use hormones and surgeries as first-line “treatment” for gender dysphoric youth.
Brilliantly demolishes every argument for “gender affirming care”. Gender medicine is a tragic example of the corruption of science by political and ideological activism. And kids are paying the price. How easily this wooly-headed, faith-based, devastatingly harmful quackery has conquered practically every major scientific institution (not to mention virtually every political party). Where were the checks and balances we all assumed would prevent such an extraordinary phenomenon? The commitment to evidence-based practice? All overcome by a toxic combination of zealotry, greed, cowardice and docility.