
An independent review of treatment for children diagnosed with gender dysphoria in the Australian state of Queensland is in the planning stages, according to the state’s Chief Psychiatrist Dr John Reilly.
Dr Reilly revealed this in reply to a letter from child and adolescent psychiatrist Dr Jillian Spencer, who is a prominent critic of the “gender-affirming” treatment model used by the Queensland Children’s Hospital gender clinic.
“It is my understanding that Children’s Health Queensland [the government agency responsible for the clinic] is planning to conduct an independent review such as you are requesting,” Dr Reilly wrote on September 21.
“In my view this is the most appropriate forum to consider the concerns that you have raised. I am not aware at present of [the] specific scope for such a review, or of [the] possible timing.”
Today Dr Spencer said: “If Queensland goes ahead with holding an independent inquiry headed by appropriately qualified and trustworthy experts who are not affiliated with the gender clinic, I will be able to sleep soundly for the first time in months.
“Queensland doctors are desperately seeking formal guidance on what interventions are safe to be delivered to children with gender dysphoria [a condition involving a sense of conflict between ‘gender identity’ and birth sex].”
Dr Spencer urged Children’s Health Queensland (CHQ) to “prevent further harm to children” by suspending puberty blocker prescriptions for new patients during the term of the independent review.
Puberty blockers are used to suppress sexual development unwanted by transgender-identifying children as young as age 10-12, typically followed by synthetic cross-sex hormones to masculinise or feminise the body. These hormones are supposed to be taken lifelong.
GCN sought comment from Queensland Health Minister Sharon Fentiman, CHQ and Dr Reilly.
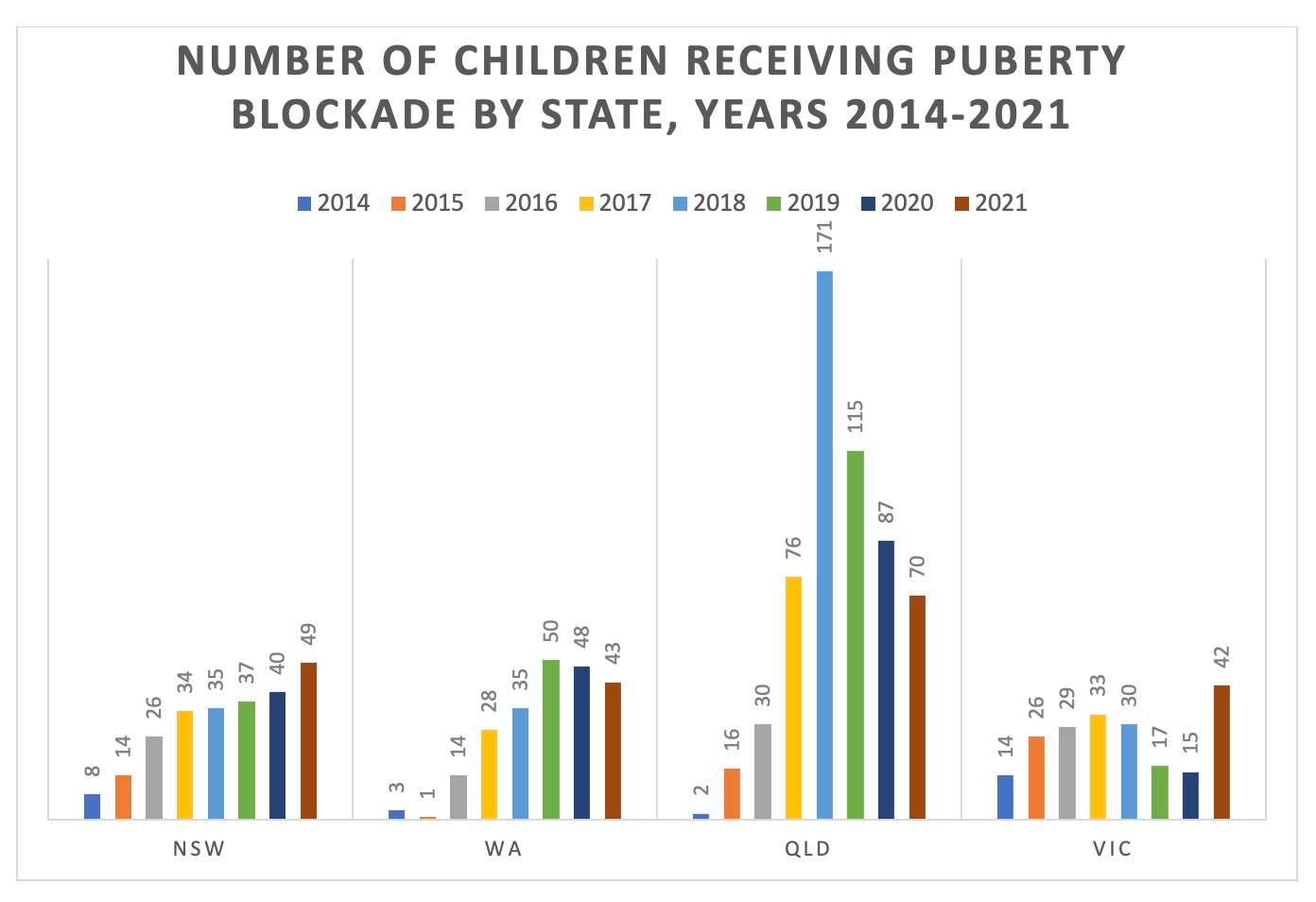
Chart: Number of children given puberty blockers by public children’s hospitals in four Australian states
Out of sync
Against the background of the European shift towards more cautious psychological approaches to gender dysphoria, Dr Spencer has raised serious concerns about puberty blockers preventing natural recovery from the distress of gender dysphoria; the sterilisation of children by hormonal treatment; uncertainty about informed consent and the risk of future lawsuits for negligence.
Following the controversy over the world’s largest gender clinic, the London-based Tavistock service, England’s National Health Service proposes to end routine treatment with poorly evidenced puberty blockers, instead confining them to formal clinical trials.
The Queensland gender clinic’s founder Dr Stephen Stathis recently acknowledged that the evidence base for the gender-affirming model’s hormonal treatments is “low quality”.
He said he no longer believed that puberty blockers offer children a “pause” before they embark upon irreversible treatment with cross-sex hormones. Data shows that almost all children started on blockers proceed to hormones.
Dr Stathis argued that if youth gender medicine were to be criticised as “experimental”, that label should also be applied to most treatments used by child and adolescent psychiatry because low-quality evidence was the norm.
Earlier this year Dr Spencer was stood down from clinical duties as a senior staff specialist at the Queensland Children’s Hospital reportedly following a complaint of “transphobia” from a young gender clinic patient.
She had tried for some months to raise safety concerns about the medicalised gender-affirming approach to treating children with gender dysphoria.
She did not work in the gender clinic but all clinical staff at her children’s hospital were under instructions to use gender-affirming pronouns and to refer gender-questioning children to the clinic. New pronouns are part of social transition—taking on an opposite-sex role—which is regarded by some clinicians as an intervention which may predispose the child to take the next, medical step.
Dr Spencer’s concerns have been amplified in media coverage by The Australian newspaper, the 7News Spotlight program and ABC Four Corners.
A total of 158 doctors so far—76 of them from Queensland—have put their names to her petition for a federal inquiry into gender clinics. Many more doctors say that fear of activist-driven reprisal prevents them expressing their concerns publicly.
In 2019, an online petition for a federal parliamentary inquiry attracted 260 doctors’ names in three days, before an activist spam attack forced its closure. This included 20 professors or associate professors, 14 paediatricians and 20 psychiatrists.
In July 2021, The Australian reported that a children’s hospital gender clinic in an unidentified state—not Queensland—was under review, with responsibility for treatment decisions shifted to family law judges. Identifying details were suppressed by the court.
The newspaper said the change followed concerns raised by a state solicitor’s office about the risk of government exposure to litigation akin to the case brought against the Tavistock clinic by detransitioner Keira Bell, a young woman who came to regret her treatment with puberty blockers, testosterone and mastectomy.
It is unclear whether that secretive Australian review has finished or has led to any change in the gender-affirming clinic’s treatment approach.
Video: “I could not hold my head up, if I didn’t speak about this”—Dr Jillian Spencer
Is consent informed?
In her August 19 letter to the chief psychiatrist, Dr Spencer wrote: “I have grave concerns regarding the assessment and treatment of children and adolescents presenting [for] care at the [Queensland Children’s Hospital and its gender clinic].”
She sought Dr Reilly’s support for an urgent independent review of “the clinical governance, including quality and safety measures, in place to ensure high quality evidence-based care can be provided to children and adolescents seeking treatment for gender dysphoria.”
She questioned whether parents giving consent to puberty blockers for their children were being adequately informed that this intervention may prevent natural recovery from gender dysphoria as children mature.
Before the rise to dominance of the gender-affirming model, multiple studies showed that the vast majority of children with early-onset dysphoria grew out of it as they developed, with many emerging as gay or lesbian adults.
In her letter to Dr Reilly, Dr Spencer said: “When puberty blockers are prescribed to a child in [early puberty around age 10-12], as is recommended by the [gender-affirming] model, and followed by cross-sex hormones, the child will be rendered permanently infertile.”
She cited the risk of future litigation and financial claims against health professionals and the hospital if hormonal treatments were continued without a proper review and remained oblivious to emerging evidence of harm.
There is international concern that the gender-affirming model discourages differential diagnosis and may medically transition young people whose mental health issues require a traditional psychotherapeutic response.
“Will the [Health Minister] intervene to restore the ability of doctors—including Dr Jillian Spencer, who has been stood down—to use their professional medical discretion when treating gender dysphoric children?”—question in Queensland’s parliament from Robbie Katter of Katter’s Australia Party, 14 September 2023
“The multidisciplinary care that hardworking clinicians provide at the children’s gender clinic is of very high quality and based on the best available evidence. This is an emerging field globally, but the evidence base is sound. I have met with a lot of families who have accessed the service at the clinic. It has been ‘life-changing’, in their words.”—answer from Queensland Health Minister Sharon Fentiman, 14 September 2023
When evidence is weak
In her letter, Dr Spencer said the Queensland gender clinic did not publish its service model, but it did reference the gender-affirming treatment guidelines first issued in 2018 by the Royal Children’s Hospital Melbourne and promoted as “Australian standards of care”.
In Finland, Sweden and England, systematic reviews of the evidence base for medicalised gender change of minors have found it to be weak and uncertain. All three jurisdictions have adopted more cautious treatment policies.
Lacking a high-quality evidence base, gender-affirming clinics rely on low-quality treatment guidelines to justify their interventions.
In its peer-reviewed version published by the Medical Journal of Australia, the RCH treatment guideline claims that, “The scarcity of high-quality published evidence on the topic [of care for dysphoric youth] prohibited the assessment of level (and quality) of evidence for these recommendations.”
“[That claim] is enough for me to say this is not a trustworthy guideline”, Professor Gordon Guyatt, a pioneer of the evidence-based movement in medicine, told GCN earlier this year.
Professor Guyatt—who is distinguished professor in the Department of Health Research Methods, Evidence, and Impact at Canada’s McMaster University—was one of the leaders in the creation of the widely used GRADE system for rating evidence quality and took part in developing the criteria necessary for a treatment guideline to be judged “trustworthy”.
The RCH guideline was considered for inclusion in the online portal Australian Clinical Practice Guidelines run by the National Health and Medical Research Council (NHMRC) but did not qualify, The Australian reported in 2021.
An NHMRC spokeswoman said: “At the screening stage it was determined that the [RCH] guideline did not include a funding statement, an evidence base for the recommendations or information about conflict of interest, and that it would not meet the portal selection criteria, so a full assessment was not carried out.”



This is very encouraging news, particularly given the requirement that the investigation is 'an independent and headed by appropriately qualified and trustworthy experts who are NOT affiliated with the gender clinic'
The reality that a multitude of scientific papers confirm that the desistance rate of gender dysphoric children is of the order of 70-80% surely should ensure that children not get sucked into the irreversible vortex that is transition.
"Dr Stathis argued that if youth gender medicine were to be criticised as “experimental”, that label should also be applied to most treatments used by child and adolescent psychiatry because low-quality evidence was the norm."
I suspect most treatments do not sterilize the young person or commit them on a pathway to lifetime hormone usage which takes their body out of normal operating conditions (with increased mortality, heart disease, immune disease, bone density harm....etc.).
The evidence of benefit is shaky if at all there beyond anecdotes but the harm is significant. It's time to start walking this back, physicians....
why do they expect their evidence review to give anything that Sweden and NICE didn't get? They're reproducible, that's the whole point....they can actually start acting on it!
Kudos and gratitude to brave Dr. Spencer! Where are the rest of the clinicians and if you are one... how are you going to explain to people in 5 years why you weren't at her side right now?