Speed offence
British paediatrician Hilary Cass puts the spotlight on Australian gender clinics racing ahead of the safety data

Into the unknown
Australian gender clinics have been criticised by England’s Cass review for using an experimental fast-track path to puberty blockers for children as young as age 8-9.
This practice could mean Australian minors stay on puberty blockers longer or start cross-sex hormones earlier, with no good data to predict safety or beneficial outcomes, according to a Cass-commissioned research paper reporting a landmark survey of international gender clinics.
“Puberty blockers [which suppress natural sex hormones] are intended to be a short-term intervention and the impact of use over an extended period of time is unknown, although the detrimental impact to bone density alone makes this concerning,” says the Cass report, noting that some patients discharged from the London-based Tavistock clinic were still on blockers in their early to mid-20s.
Australia’s health ministers and gender clinicians have sought to deny the local relevance of the Cass report by making vague claims about different pathways to treatment in the two countries. However, Australia’s gender clinics loom large in research commissioned by Dr Cass, especially in a survey of 15 international clinics and an independent evaluation of 21 treatment guidelines around the world.
In the newly published guideline research, not one of the three reviewers recommended use of the 2018 “Australian standards of care” treatment guideline issued by the Royal Children’s Hospital (RCH) Melbourne1.
The RCH guideline scored only 19/100 for the rigour of its development, compared with 71/100 for the more cautious and up-to-date treatment advice from Sweden. The RCH guideline—judged untrustworthy by a pioneer of evidence-based medicine, Professor Gordon Guyatt—is used by Australia’s children’s hospital gender clinics and the stand-alone Maple Leaf House clinic.
In the Cass-commissioned survey, the majority of the international clinics that responded said they did not routinely collect outcome data on their young patients. Clinics were listed by country, not name, although clues in survey responses identify some clinics. Australia had the largest number of clinics—five of the 15—in the survey.
The research paper reporting the 2022-23 survey—published in the BMJ’s Archives of Disease in Childhood—highlights the fact that three Australian gender clinics offer a “unique” pathway for “peri-pubertal” children who are given priority on the waiting list for psychological support and access to puberty blockers when eligible.
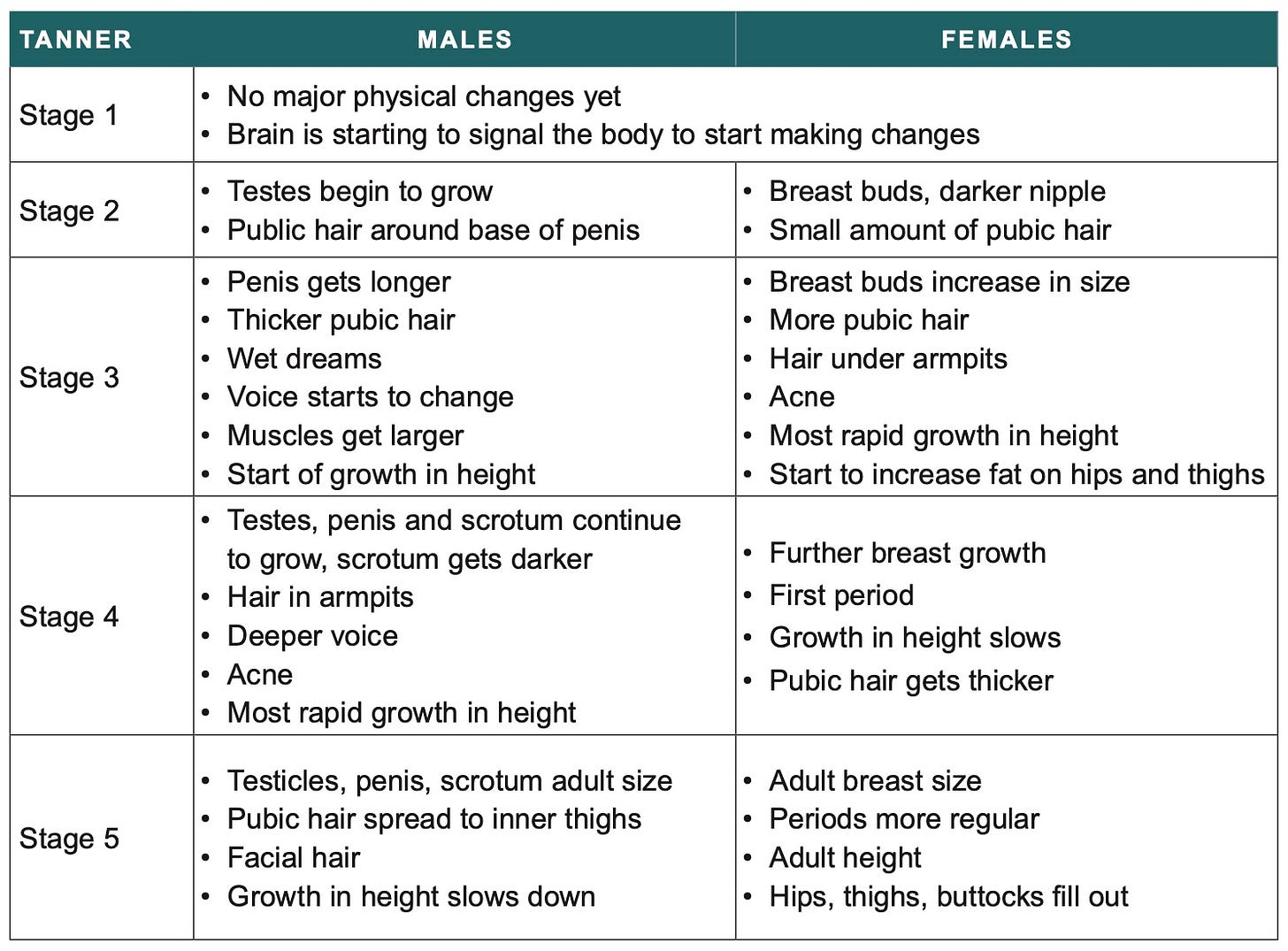
The paper says the age of entry to this pathway is 8-9, as early as Tanner Stage 1; Tanner Stage 2 marks the onset of puberty.
Answers to survey questions identify the three fast-track clinics as those of the Perth Children’s Hospital2, the Queensland Children’s Hospital and RCH (which appears most responsible for entrenching the contentious “gender-affirming” treatment approach in Australia.)
In a 2018 journal article, the RCH clinic authors describe the setting up of its “innovative” single-session nurse-led assessment clinic, stating that this new “system enables those patients who will benefit most from puberty-blocking treatment to be fast tracked into the multidisciplinary assessment pathway to access treatment as required.”
The Queensland gender clinic had the shortest waiting time in the Cass survey, with just two to three appointments over two to three months3.
Writing in the BMJ earlier this month, Dr Cass said: “The rationale for early puberty suppression remains unclear, with weak evidence regarding the impact on gender dysphoria and mental or psychosocial health. The effect on cognitive and psychosexual development remains unknown.”
Chart: Puberty by Tanner stage. Credit: Cass report
No outcome data
The survey research paper, authored by University of York researchers commissioned by Dr Cass, notes that the Australian fast-track to puberty blockers is supported by the 2018 RCH treatment guideline for youth gender dysphoria.
But the York paper points out that “the impact of this [fast-track pathway], which might entail longer use of interventions to suppress puberty or earlier commencement of masculinising/feminising hormones, remains unknown4 as early studies of outcomes of interventions to suppress puberty mandated a minimum age of 12.”
“Traditionally, ‘watchful waiting’ has been recommended to observe how gender feelings and any distress develops [in pre-pubertal children], as the evidence suggests that many children’s gender questions or concerns may not persist into adolescence.”
In 2019, RCH head of research Dr Ken Pang advertised a PhD project on the unknown effects of hormone suppression on the brain, stating “this use of puberty blocking medication typically occurs for several years”5.
A 2020 journal article, with RCH gender clinicians and University of Melbourne bioethicists among the authors, considers the case of 15-year-old male child “EF”, a hypothetical “non-binary” patient combining features of real cases.
After three years of hormone suppression EF’s bone mineral density has fallen to the lowest 2.5 percentile, “although there have been no fractures,” the authors say.
“EF, whose desire for biological children in the future remains unclear, wishes to continue puberty suppression until they are at least 18 years old [thereby keeping a seemingly androgynous body]. Their clinicians contact the clinical ethics consultation team to ask, ‘Is that appropriate?’”
The paper assumes, contrary to systematic reviews of the evidence, that blockers can be counted on to ease the distress of gender dysphoria and confer mental health benefits. In other words, the paper does not accept that the use of blockers with dysphoria is experimental6.
Three of the Melbourne authors suggest the “attractive” option of maintaining EF on blockers while making experimental use of another medication. They say that “selective estrogen receptor modulators” (SERMs) might “theoretically promote improved bone density” without growing undesired breast tissue. It is “attractive”, they suggest, despite this new medication’s side effects including hot flashes, blood clots and possibly cognitive impairment.
Another 2020 paper involving authors from the RCH clinic and the University of Melbourne contemplates the composite case of “Phoenix”, a non-binary adult requesting ongoing puberty suppression (OPS) to permanently prevent the development of secondary sex characteristics, as a way of affirming their gender identity.”
The hypothetical Phoenix is an 18-year-old girl who has mostly identified as non-binary and began hormone suppression at age 11 after she became “extremely distressed” by the appearance of breast buds and the thought of approaching menarche.
The authors declare perpetual puberty blockers “ethically justifiable”, because the possible harms would be outweighed by benefits such as “a physical appearance that better matches gender identity.”
“We have also contended that Phoenix’s request can be regarded as substantially autonomous. Arguably, medicine is moving beyond its traditional, narrow goal of promoting health, biostatistically conceived.”
Under the rubric of more ethical work to be done with non-binary adults, the authors ask, “Should a diagnosis of gender dysphoria be required for an individual to be eligible for puberty suppression?”
All this is in stark contrast to the Cass report, which says—“Puberty suppression was never intended to continue for extended periods, so the complex circumstances in which young people may remain on puberty blockers into adulthood is of concern.”
“In some instances, it appears that young adults are reluctant to stop taking puberty blockers, either because they wish to continue as non-binary, or because of ongoing indecision about proceeding to masculinising or feminising hormones.”
But the Cass report warns that “a known side effect of puberty blockers on mood is that it may reduce psychological functioning.”
“Even at Tanner stages 2-3 [roughly ages 9-13], young people have had minimal experience of their own biological puberty, and such experience as they have had may have been distressing for a wide range of reasons.
“Once on puberty blockers, they will enter a period when peers are developing physically and sexually whilst they will not be, and they may be experiencing the side effects of the blocker. There are no good studies on the psychological, psychosexual and developmental impact of this period of divergence from peers.
“However, if a young person is already on puberty blockers, they will need to make the decision to consent to masculinising [or] feminising hormones at a point when their psychosexual development has been paused, and possibly with little experience of their biological puberty.”
Video: Helen Joyce of the UK gender-critical group Sex Matters discusses the Cass report with John Anderson, a former deputy prime minister of Australia
Misguideline
In their paper on the survey of international gender clinics, the University of York authors note that the RCH treatment guideline—used by gender clinicians in Australia’s children’s hospitals and the Maple Leaf House clinic in regional NSW—had abandoned key safeguards of the 2011-14 “Dutch protocol” studies which provide the evidence base for gender medicalisation with puberty blockers, cross-sex hormones and surgery.
Unlike the original Dutch protocol, the RCH guideline does not restrict this medicalisation to patients with gender dysphoria since early childhood who are otherwise psychologically stable. The RCH document says psychosis, depression and anxiety are not necessary barriers to starting minors on life-altering hormonal treatment which can cause sterilisation, sexual dysfunction and other poor health outcomes.
The York researchers contrast the radical RCH guideline with Finland’s more cautious 2020 treatment policy, which returned to the stricter Dutch approach after clinicians noted the poor outcomes for patients with adolescent-onset dysphoria, this being the typical case profile since around 2015. (The Dutch studies, still considered the best available evidence, have recently come under closer scrutiny for their shortcomings.)
Only the Finnish and Swedish 2022 guidelines—which recognise the very weak evidence base confirmed by systematic reviews—were recommended by the Cass report following the evaluation run by the York researchers.
The Swedish guideline was rated 71/100 for the rigour of its development and Finland’s score for rigour was 51, while the RCH guideline scored 19. The rating for the Endocrine Society’s 2017 guideline was 42 and the rigour score for the 2022 standards of care from the World Professional Association for Transgender Health (WPATH) was 35.
For editorial independence, the scores were 14 for RCH, 39 for WPATH and 92 for the Endocrine Society.
Australia’s health authorities typically invoke three guidelines—from RCH, the Endocrine Society and WPATH—when giving public assurances about the quality and safety of care at gender clinics.
Citing the low quality of most treatment guidelines, the Cass report recommends that “healthcare services and professionals” adopt a cautious approach7.
GCN put questions to the health authorities responsible for the gender clinics at the Royal Children’s Hospital Melbourne, the Queensland Children’s Hospital and the Perth Children’s Hospital
Although the RCH treatment guideline is badged as “Version 1.4 (2023)”, its 70-item reference list does not include any studies after 2018. Since 2019, a number of European countries have published the results of independent systematic reviews of the evidence base—the gold standard for testing the quality of data said to support treatment—for paediatric gender medicine.
Some 2021-22 decisions of the Family Court of Western Australia approving puberty blockers for minors recite the claim that “the effects of this treatment are reversible when used for a limited time for approximately three to four years.” That claim is attributed to the 2017 re Kelvin decision of Australia’s Family Court, which in turn seems to have relied on a draft copy of the 2018 RCH guideline and an affidavit of the RCH clinic director Dr Michelle Telfer. However, the guideline itself does not give a time limit after which the effects of puberty blockers may be irreversible.
Whistleblower psychiatrist Jillian Spencer lodged a complaint with Queensland’s Office of the Health Ombudsman when she became aware that a troubled child had been prescribed puberty blockers after only two appointments at the state’s gender clinic. The ombudsman took no action, according to Dr Spencer.
The risky lowering of the minimum age for puberty blockers at the London-based Tavistock clinic is a key theme of the Cass report. Under paediatrician Russell Viner, the Tavistock’s “early intervention” study recruited children from age 12. Although preliminary data from the study was not encouraging, the Tavistock in 2014 rolled out early blockers as routine treatment without emulating the more careful patient selection of the original Dutch protocol. In 2016, RCH gender clinic nurse Donna Eade visited Professor Viner in London to learn about the Tavistock model, thanks to the $50,000 Dame Elisabeth Murdoch nursing scholarship. Ms Eade was accompanied by the RCH clinic director, Dr Michelle Telfer. At the time, full results of the Tavistock’s early intervention study remained unpublished. As for RCH, it had already given puberty blockers to a (physically advanced) 10-year-old child known as “Jamie”, following a 2013 appeal court ruling. The trial judge had noted the reassurances offered by a senior endocrinologist, identified only as “Dr G”. The judge wrote: “Dr G saw no problems in carrying out the first stage of treatment [being puberty suppression]. It is fully reversible. It has no side effects. As he said, ‘Endocrinologists have been prescribing it for years in children much younger than [Jamie], to arrest precocious puberty’. It would enable Jamie’s mental development to proceed ‘normally’, without the ‘terrible impediment’ of gender dysphoria.” None of these reassurances survives scrutiny after the Cass report.
A 10-year review at the RCH gender clinic—covering patients first seen between 2007 and 2016—did not report any data on the duration of puberty blocking treatment. The authors of the resulting journal article noted that “pubertal status was not always uniformly documented in the clinical notes and was therefore not extracted or analysed”. The review did not capture the recent dramatic growth in patient numbers. From 2007-2013, the clinic had less than 100 new referrals; from 2014-2020 there were 1,830 new referrals.
Public health authorities in Finland, Sweden, and England have concluded, explicitly or implicitly, that the use of puberty blockers for gender dysphoria is experimental and should be confined to ethically controlled clinical trials.
The Cass report says it is “imperative” that gender clinic staff be “cognisant of the limitations in relation to the evidence base and fully understand the knowns and the unknowns.”



I find it difficult to conjure up a medical intervention that is more unacceptable and inappropriate than that of the affirmative model of ‘treating’ gender dysphoria (GD) in children.
I cite a few of the many arguments against this dreadful detour down a medical abyss:
• It is not evidence based.
• Some 80% of children presenting with GD will ‘desist’ (no longer experience the distress of GD following puberty) and there is no way to determine which 20% would ‘persist’ with GD.
• It impacts a cohort already heavily burdened with mental health challenges prior to emergence of the GD.
• Children given of-label drugs with unknown long term effects.
• Children are surgically mutilated and irreversibly sterilised.
• It is banned in ever more countries in Europe (those that originally pioneered the model) and much of the Western World.
• Medical defence for medical practitioners is withdrawn in ever more locations.
• Despite the insistence of protagonists as to the positive outcomes following ‘gender reassignment’, studies of long-term outcome (10 to 20 years) indicate a higher rate mental health issues and suicide.
"... Arguably, medicine is moving beyond its traditional, narrow goal of promoting health, biostatistically conceived.”
Good Lord. I guess "first do no harm" is also becoming quaint and parochial.
It seems to me that, at its heart, the war being waged isn't just for the health and welfare of our children, but for science against pseudo-scientific and anti-scientific mysticism. The "critical theory" juggernaut is pure fraud. It needs to be said, loudly and frequently, that there ARE no "other ways of knowing".