Risky business
Australian politician Moira Deeming says it's time to rethink youth gender medicine

Australian politician Moira Deeming has called for an urgent review of irreversible medical treatments for minors who reject their birth sex and identify as transgender or non-binary.
She cited two red flags in the form of a major medical indemnity fund, MDA National, cutting back its cover for youth gender medicine, and family law barrister Belle Lane’s warning to the judiciary on the risks of the “gender-affirming” treatment approach.
“Will the government take responsibility and call for an urgent inquiry to review social, medical and surgical gender-transition practices on minors in Victoria”, Mrs Deeming said in state parliament earlier today.
In the adjournment debate, she suggested the inquiry also should look at the indemnity insurance risk carried by taxpayers and Victoria’s Labor government, which is responsible for Australia’s most influential gender-affirming clinic at the public Royal Children’s Hospital Melbourne.
And Mrs Deeming asked Education Minister Natalie Hutchins how many children in Victoria’s public schools had been declared “mature minors” to enable their social transitioning, and how state education policy and curriculum showed respect for parental rights.
A mature minor is considered capable of making autonomous decisions, although the application of this concept to gender change is contentious.
The practice of schools enabling or promoting social transition—whereby the child lives out a cross-sex role with a new name and identity—without seeking consent from parents is emerging as a fierce controversy in rich countries around the world.
In Victoria, government education policy says: “If a student is considered a mature minor they can make decisions for themselves without parental consent and should be affirmed in their gender identity at school without a family representative/carer participating in formulating the school management plan.”
Mrs Deeming, who was expelled from the opposition Liberal Party after she attended March’s Let Women Speak rally in Melbourne, sits on the crossbench and continues to pursue her longstanding interest in the welfare of women and children.)
Video: Moira Deeming urges an inquiry into youth gender clinics
Roadblock ahead
Attempts to fast-track and mainstream cross-sex hormones for trans-identifying minors will come under pressure if more medical indemnity firms conclude that they face an increasing risk of treatment regret and litigation.
From July 1, the indemnity insurer MDA National will restrict coverage of claims against private practitioner members involved in starting minors on cross-sex hormones or assessing them as ready for “gender transition.”
“We consider it appropriate that the assessment and initial prescribing for patients transitioning under the age of 18 years occurs with the support and management of a multi-disciplinary team in a hospital setting,” MDA National said in an email to doctors explaining the new policy.
Although other indemnity firms have told doctors they do not plan similar restrictions, gender-affirming clinicians are worried about the possible spread of the perception that hormonal interventions with minors carry an elevated medico-legal risk.
Twitter: In 2019 GP Fiona Bisshop, who went on to serve as president of the Australian Professional Association for Trans Health, expressed a view shared by other gender clinicians: that hormones can safely be given in primary care
Watch this space
The large national indemnity insurer Avant has answered questions from inquiring doctors by saying its underwriters propose no change to coverage “at present.”
GCN understands that Avant is the indemnity fund for psychiatrist Dr Patrick Toohey in the negligence claim brought by detransitioner Jay Langadinos. This case in the NSW Supreme Court is in its early stages and has a directions hearing scheduled for June 7.
Detransitioners who regret treatment have also begun litigation in the United States and United Kingdom.
Last year, Avant’s head of medico-legal advice Kate Gillman addressed a scientific meeting of the NSW Medico-Legal Society in Sydney on the topic “Gender dysphoria—transgender children.” Her experience includes work with a London law firm specialising in medical negligence litigation for the National Health Service.
Two other Australian medical indemnity funds, MIPS and MIGA, told GCN they had made no changes to their coverage of gender medicine. Tego, the remaining firm, did not reply to requests for comment.
New referrals to the gender clinic at the Royal Children’s Hospital Melbourne rose from eight in 2011 to 821 in 2021. Some basic data has been obtained from other children’s hospital clinics elsewhere in Australia but there are no comprehensive statistics available.
In her dossier for family law judges, barrister Belle Lane points out that the total number of young people given gender medicine by public clinics, private clinics and suburban doctors is “unknown”, and nor is there proper data on treatments and outcomes.
“This presents a significant problem for research and is particularly concerning considering the long-term medical implications of endocrine treatment [such as cross-sex hormones],” Ms Lane says.
Video: “It was only a month after my 13th birthday that I had a double mastectomy”
On the gender beat
Following GCN’s May 9 breaking news report of MDA National’s plan to restrict cover for aspects of youth gender treatment, the story has been picked up by mainstream media and the medical press, thereby increasing speculation.
The web magazine The Medical Republic covered the news with a headline suggesting MDA National was “transphobic”—a claim later denied by the indemnity firm—and an image of a man with a pistol.
Media studies: a puzzling image choice by The Medical Republic
Long tail of regret
In the report by newsGP, an outlet of the Royal Australian College of General Practitioners, MDA National president Dr Michael Gannon said that, “One of the problems with long-tail insurance is that you might make a decision, or there might be a clinical matter that’s dealt with, and then it takes five, 10, 15, 20 years before that turns into a clinical problem.”
Studies suggest that regret may lag gender treatment by a decade, and historically low rates of regrets cited by clinicians seeking to reassure sceptics may not apply to today’s altered patient profile reportedly given less cautious assessments.
“We’re talking about people who are making life-changing decisions,” Dr Gannon said. “So, our feeling is that that is a very high level of risk for an individual GP [a general practitioner or family doctor] to take on their own.”
He said the change of policy had generated “a lot more positive than negative feedback from our members who felt unsafe prescribing some of these hormones. They felt pressured to prescribe hormones in an area that they didn’t quite understand…”
Dr Gannon, a former president of the Australian Medical Association and chair of its ethics and medico-legal committee, also cited the controversy over the London-based Tavistock gender clinic as an influence in the insurer’s adoption of a more cautious position.
A case of nerves
Quite apart from the risk of personal liability in negligence claims, some GPs already have expressed a lack of confidence about the process and legality of initiating cross-sex hormones with minors.
Gender-affirming clinicians and activists urge the mainstreaming of this treatment in primary care to meet demand from post-pubertal teens caught between crowded gender clinics at public children’s hospitals and adult services.
There are anecdotal reports of teens as young as age 14 being put on synthetic hormones without a mental health assessment, a safeguard which might indicate underlying non-gender issues as the true priority for treatment.
GCN asked the regulator, the Australian Health Practitioner Regulation Agency, for details of any complaints against clinicians over medical transition of minors or assessment for transition.
“As our database does not categorise cases according to these criteria or terms, we are not able to provide overall statistics within this timeframe,” an Ahpra spokesperson said.
After the September 2020 ruling by the Family Court in the re Imogen case, the TransHub website run by ACON—formerly a gay health agency but now a de facto trans activist lobby—was forced to correct advice favouring the fast-tracking of lifelong cross-sex hormones for patients from the age of 16.
In July 2020, the Australian Journal of General Practice ran an article by a GP arguing that in most cases cross-sex hormones could be given to patients at age 16 in a primary care setting without the need for a formal diagnosis of gender dysphoria by a mental health specialist.
This was legally incorrect, according to a July 2021 opinion piece by legal academic Professor Patrick Parkinson and Dr Philip Morris, president of the National Association for Practising Psychiatrists. (The NAPP has published a cautious guide to youth gender care.)
Their article in a web magazine affiliated with the Medical Journal of Australia set out three conditions for lawful prescription of hormones to minors—
a formal diagnosis of gender dysphoria
treatment in line with established guidelines, which require the involvement of a multidisciplinary team
the agreement of both parents
Sliding doors
Youth gender clinics in the public health system may be indirectly affected by the new MDA National policy if they rely on part-time practitioners—such as an endocrinologist, paediatrician or psychiatrist—who would normally be expected to rely on their own indemnity insurance rather than the hospital’s in the event of a claim such as a negligence action.
“They’re going to have to work out if they’re covered by the government for their work in the clinic,” said the NAPP’s Dr Morris.
“There is an issue that may be of great concern.”
He said that doctors who were full-time employees in the public system would normally be indemnified by the hospital against claims arising from a genuine mistake, as opposed to conduct that was criminal or well outside normal clinical standards.
Another uncertainty is the insurance coverage of medical practitioners working for the Orygen-headspace mental health network.
“At headspace, everyone is responsible for their own clinical indemnity,” one health practitioner familiar with the service told GCN, speaking on condition of anonymity.
“Only a small minority would be doing the work that is not covered [by MDA National], but the messaging is sobering for those that might have been tempted.”
In 2021, the state government of Victoria budgeted $21million “to support the mental health of trans and gender-diverse young people”, including the establishment of a “clinical pathway” from the gender clinic at the Royal Children’s Hospital Melbourne (RCH) to Orygen.
RCH and the lobby groups Transcend and Transgender Victoria are partners in the new Orygen Trans and Gender Diverse Service.
This service is intended to be statewide and aimed at patients aged 12-25 with gender dysphoria or other gender identity issues. It will offer assessment, treatment and support in line with the 2018 RCH treatment guideline, according to Orygens documents.
Note: GCN sought comment from the Australian Professional Association for Trans Health, Orygen, headspace, Victoria’s Health Minister, and The Medical Republic


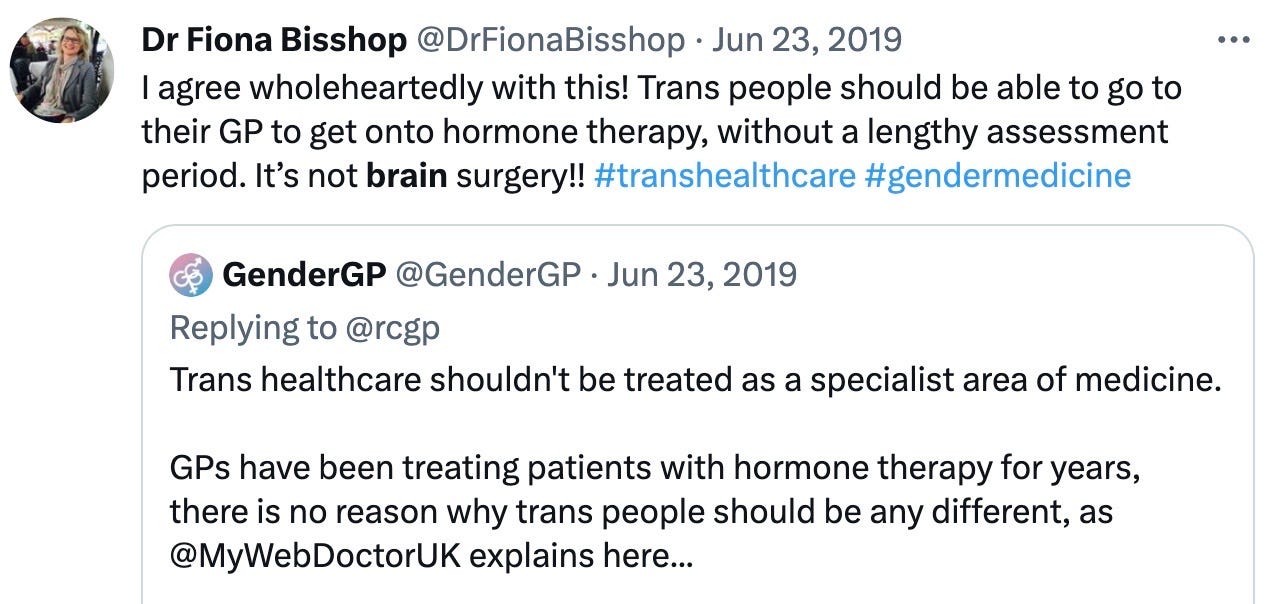

General practitioner Dr Fiona Bisshop’s comment “Trans people should be able to go to their GP to get onto hormone therapy without a lengthy assessment period. It’s not brain surgery” does little to instil confidence into the safety and protection of the vulnerable.
Endocrinology and psychiatry are complex and highly specialised fields in medicine and
there remains a great deal of concern among relevant specialists as to the appropriateness of irreversible, sterilising and mutilating procedures in young people.
I believe that for a general practitioner to suggest that “it’s not brain surgery” in the face of the reality is trivialising a dreadful reality.
Further evidence of the way medicine and the counselling professions can be swept away by dangerous quackery and activism. I chose to resign from my professional counselling body PACFA (Psychotherapy and Counselling Federation of Australia) because they were censoring discussions on their private members-only forums regarding the harms of transitioning minors. Even the word “detransitioner” was unmentionable. Their explanation?: Such conversations made the “gender diverse” people on one of their internal bodies feel “unsafe”. When the delicate sensibilities of counsellors matter more than the minds, bodies and futures of vulnerable young people, something’s gone terribly wrong: the moral compass that should be operating has broken.