One-way treatment
The famous Dutch clinic admits that puberty blockers may be a prediction, not a pause

The gist
The Dutch gender clinic that pioneered the use of puberty blockers has conceded that children taking these drugs may find themselves locked in to more medicalisation.
The promise of being able to stop an unwanted puberty has driven an international surge in demand for gender medicine since the 2010s, especially from teenage females with a range of other problems.
In a retrospective study of 1,766 children and adolescents between 1972 and 2018 at the famous Amsterdam clinic, researchers earlier this month reported that 93 per cent of eligible patients on puberty blockers went on to take opposite-sex hormone drugs.
The Dutch had argued that blockers were fully reversible and afforded patients, families and practitioners a distress-free breathing space to clarify diagnosis, explore gender identity and consider the next step to partly irreversible opposite-sex hormones. Variations on this rationale are still offered internationally by gender clinicians and transgender rights activists.
However, the new Dutch retrospective paper confirms the finding of three recent studies since 2018 that the vast majority of those who begin on blockers proceed to opposite-sex hormones.
This is a treatment combination expected to sterilise these young people if they are set upon the medical path early in puberty; it implies that children as young as age 8-9 are capable of giving informed consent to a lifelong medical pathway.
The new paper published in The Journal of Sexual Medicine reviewing 20 years of the hormonal interventions known as the “Dutch protocol” includes authors associated with this 1990s medical innovation, but it does not repeat the familiar claim that puberty blockers are reversible.
The paper by endocrinologist Dr Maria A.T.C. van der Loos and colleagues says the finding that blockers at the Amsterdam clinic almost always led to opposite-sex hormones “may imply that [puberty blocker] treatment is used as a start of transition rather than an extension of the diagnostic phase.”
The researchers suggest that most patients who began blockers in the study must have suffered “sustained” gender dysphoria, a distressing sense of conflict between birth sex and an inner gender identity.
“Still, one cannot exclude the possibility that starting [puberty blockers] in itself makes adolescents more likely to continue medical transition,” the paper warns.
This is the “biggest admission” yet that puberty blockers are not reversible nor a diagnostic tool, according to University of Oxford sociologist Dr Michael Biggs, who published a detailed critique of the Dutch protocol treatments last September.
“At last the Dutch clinicians are finally admitting what many of us have been saying for years, that puberty blockers — and social transition [living as if the opposite sex] — become a self-fulfilling prophecy,” Dr Biggs told GCN.
“The Amsterdam clinic has been manufacturing 'juvenile transsexuals’ — to quote the original Dutch article from 1996).”
One of the authors of the new retrospective study, the prominent child psychiatrist Dr Annelou de Vries, was asked in the Dutch media earlier this month if puberty blockers were a “self-fulfilling prophecy” pushing young patients onwards to opposite-sex hormones.
She replied: “You can also turn it around. We look very carefully at who we give puberty blockers to, and those are indeed the young people with a very high chance that [opposite-sex identity] is not a temporary whim. Apparently, we can make that selection well.”
England’s independent review of youth gender care, led by paediatrician Dr Hilary Cass, has drawn attention to a troubling uncertainty about the real purpose of puberty blockers, with clinicians shifting rationales.
Known as gonadotropin-releasing hormone analogues (GnRHa), the hormone suppression drugs adopted by gender clinics as puberty blockers have regulatory approval for other conditions including precocious puberty, prostate cancer and endometriosis. They are also used for “chemical castration” of sex offenders.
Video: Psychiatrist Dr Az Hakeem on puberty blocker myths
The detail
The new Dutch paper by van der Loos and colleagues concludes that its retrospective review of patient charts “in a large cohort over an unprecedented time span” offers “ongoing support for medical interventions in comprehensively assessed gender diverse adolescents.”
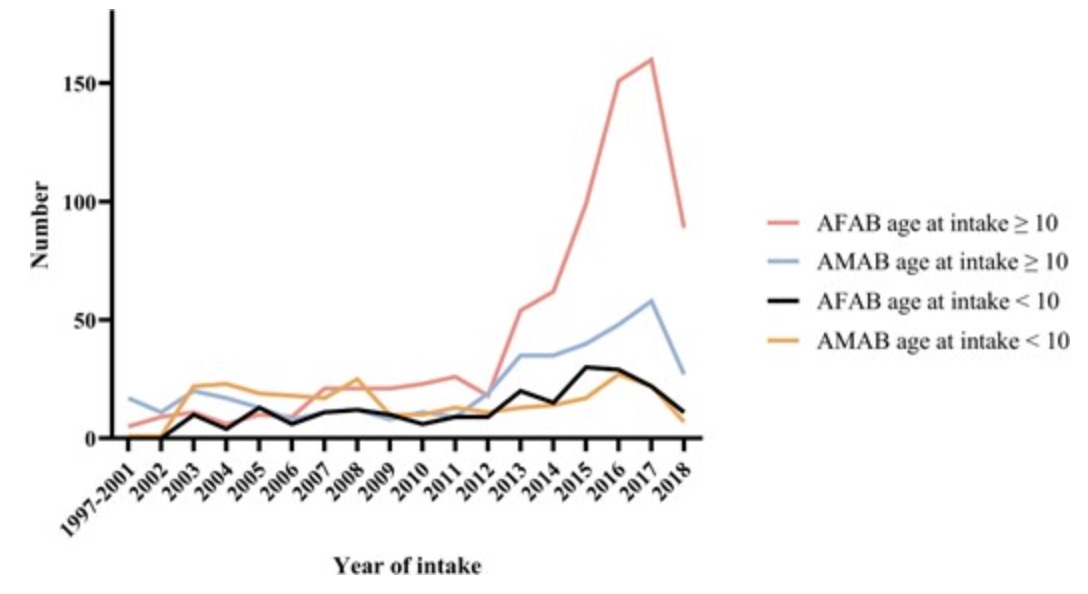
The data confirms that the Amsterdam clinic too has witnessed the poorly understood international shift in dysphoric patients from males to females, with “overwhelming demand” leading to a restricted number of new referrals from 2018 onwards at the clinic.
The paper reports a “remarkable” sex difference in hormone suppression. Of eligible female patients, 73 per cent began puberty blockers; the figure for males was 47 per cent. The authors suggest that dysphoria may be “more severe” in females but admit the need for “more compelling” explanations.
They acknowledge that the reported rates of medical treatment in the recent period of rapid growth in patient numbers are likely to be “an underestimation”, with potentially many patients starting hormonal interventions after the end of data collection in 2018.
Oxford University’s Dr Biggs said the new paper also revealed a trend of increasing use of puberty blockers among those patients who came to the clinic under the age of 10.
“That accords with the finding from other research from this clinic that prepubertal social transition has increased — even though the Dutch advised against it — and that it becomes a self-fulfilling prophecy,” he said.
Chart: Patient demand at the Amsterdam clinic
Regrets
The van der Loos paper reports that detransition was “very rare” but acknowledges data might be missing as a result of the retrospective research design. The median time for follow-up was 4.6 years, the short duration perhaps reflecting the large number of recent patients in the study.
A recent paper critical of the Dutch protocol argues that with the international expansion of gender medicine, the rate of regretful detransition “appears to be accelerating.”
This paper by American psychiatrist Dr Stephen B. Levine and colleagues cites various measures of detransition — or findings suggestive of detransition — which would indicate a rate of at least 10 per cent of patients stopping treatment.
“Given that regret may take up to 8-11 years to materialize, many more detransitioners are likely to emerge in the coming years,” the paper says.
A study of 100 detransitioners by American public health researcher Dr Lisa Littman reported that only 24 had told their former gender clinicians that they had detransitioned.


Gay conversion therapy?
In his 2022 analysis of the Dutch protocol, Oxford’s Dr Biggs said it was “plausible” for the Amsterdam clinic to have justified the innovation of puberty blockers as a diagnostic tool that enabled exploration of gender identity.
“It was also plausible that stopping normal cognitive, emotional, and sexual development would impede such exploration,” his paper says.
In truth, he argues, puberty blockers were not diagnostic because the vast majority of patients given them went on to opposite-sex hormones, and the claim of reversibility was undermined from the start by the still unknown effect of hormone suppression on the developing adolescent brain.
The Biggs paper says the framing of blockers as diagnostic “circumvented a problem” that had been recognised early in the medical literature of the Dutch protocol.
Those early papers had cited studies reporting that feminine boys diagnosed with “gender identity disorder” — as gender dysphoria used to be known — were more likely to grow up as homosexuals, not transsexuals.
“These findings were downplayed in subsequent publications [from the Amsterdam clinic]; the key manifestos for the Dutch protocol did not mention homosexuality and did not cite any study of feminine boys,” Dr Biggs says.
“Of the first 70 adolescents referred to the Amsterdam clinic from 2000 to 2008 and given [puberty blockers], 62 were homosexual while only one was heterosexual.
“Clinicians need to explain how they are sure that some of the adolescents being prescribed [puberty blockers] would not have grown into gay or lesbian adults, with their sexuality and fertility intact.”
The same concern surfaced in the 2015 Dutch “empirical ethical” study, which surveyed 36 clinicians and academics in 10 countries — including child and adolescent psychiatrists, psychologists, endocrinologists and ethicists — on the contentious issue of hormonal intervention early in puberty.
The study revealed seven dimensions of profound disagreement over hormonal suppression, such as the role of puberty in developing gender identity and the competence of children to authorise treatment.
The authors, who included well-known Dutch clinicians, said: “Concerns have been raised about the risk of making the wrong treatment decisions and the potential adverse effects on health and on psychological and psychosexual functioning.”
“I have met gay women who identify as women who would certainly have been diagnosed gender dysphoric as children but who, throughout adolescence, came to accept themselves. This might not have happened on puberty blockers.” — said one of the psychologists surveyed
“You might think that the experience of gender dysphoria is kind of a solution [for all their problems] that is culturally available for adolescents nowadays. I think that the culture is kind of offering or allowing this idea that all problems are stemming from the gender problem. And then they stick to this fixated idea and [they] seek for assessment and we readily see that they have numerous and relatively serious psychological and developmental problems and mental health disorders.” — a psychiatrist
“More and more treatment teams embrace the Dutch protocol but with a feeling of unease. The professionals recognize the distress of gender dysphoric youth and feel the urge to treat them. At the same time, most of these professionals also have doubts because of the lack of long-term physical and psychological outcomes.” — the study’s authors
Sexuality needs puberty
A 2008 paper by the prominent German child and adolescent psychiatrist Dr Alexander Korte and colleagues also argued that early hormonal intervention was fraught with risks.
“As children with [gender identity disorder] only rarely go on to have permanent transsexualism, irreversible physical interventions are clearly not indicated until after the individual’s psychosexual development is complete,” the paper said.
“The identity-creating experiences of this phase of development should not be restricted by the use of [hormone suppression drugs] that prevent puberty.
“Multiple longitudinal studies provide evidence that gender-atypical behavior in childhood often leads to a homosexual orientation in adulthood, but only in 2.5 per cent to 20 per cent of cases to a persistent gender identity disorder.
“Most advocates of early hormonal intervention assert that the effects of puberty-blocking treatment are totally reversible. This is true, however, only with respect to its physical effects, not with respect to the irreversible damage it does to the process of psychosexual development.”
The authors cited the experience of a Berlin gender clinic with 21 young patients where “the motive for switching” to an opposite-sex identity was judged to be mainly “a rejected homosexual orientation, the development of which would have been arrested by puberty-blocking treatments.”
They warned that blockers restricted sexual appetite and denied patients age-appropriate sexual experiences, making it “nearly impossible [for them] to discover the sexual preference structure and ultimate gender identity [that develops] under the influence of the native sex hormones.”
They said it was unclear whether hormonal intervention before the end of puberty might prolong the distress of gender identity disorder, making this potentially a case of iatrogenic medicine.
“Even in a case of treatment retrospectively judged to have been successful, one cannot necessarily assume that the patient’s transsexualism was a predetermined matter at the outset,” they said.


The failure of researchers proposing the early intervention study at the Tavistock to include a control group led an ethics approval committee to withhold approval. The researchers got clearance from a second ethics committee (as the rules allowed).
It is difficult to believe that history will be kind to those promoting invasive, irreversible, sterilising ‘gender change’ in young people.
The arguments in favour of continuing on this pathway are becoming ever less plausible with much of the initial supportive ‘science’ eroded.
Also of concern is that many of the practitioners involved in the process of ‘transition’ are also campaigning politically for support of the interventions. This is an inappropriate invasion a domain that should be based on sound, irrevocable science, by which I mean satisfaction of the gold standard clinical trial.